Influenza and COVID-19 are respiratory diseases caused by the influenza virus and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and share clinical risk factors and symptoms. However, the extent of their shared genetic etiology remains unclear because the host genetic risk factors for COVID-19 are well characterized but not for influenza. Identifying common genetic risk factors could reveal targets to treat or prevent both infections.
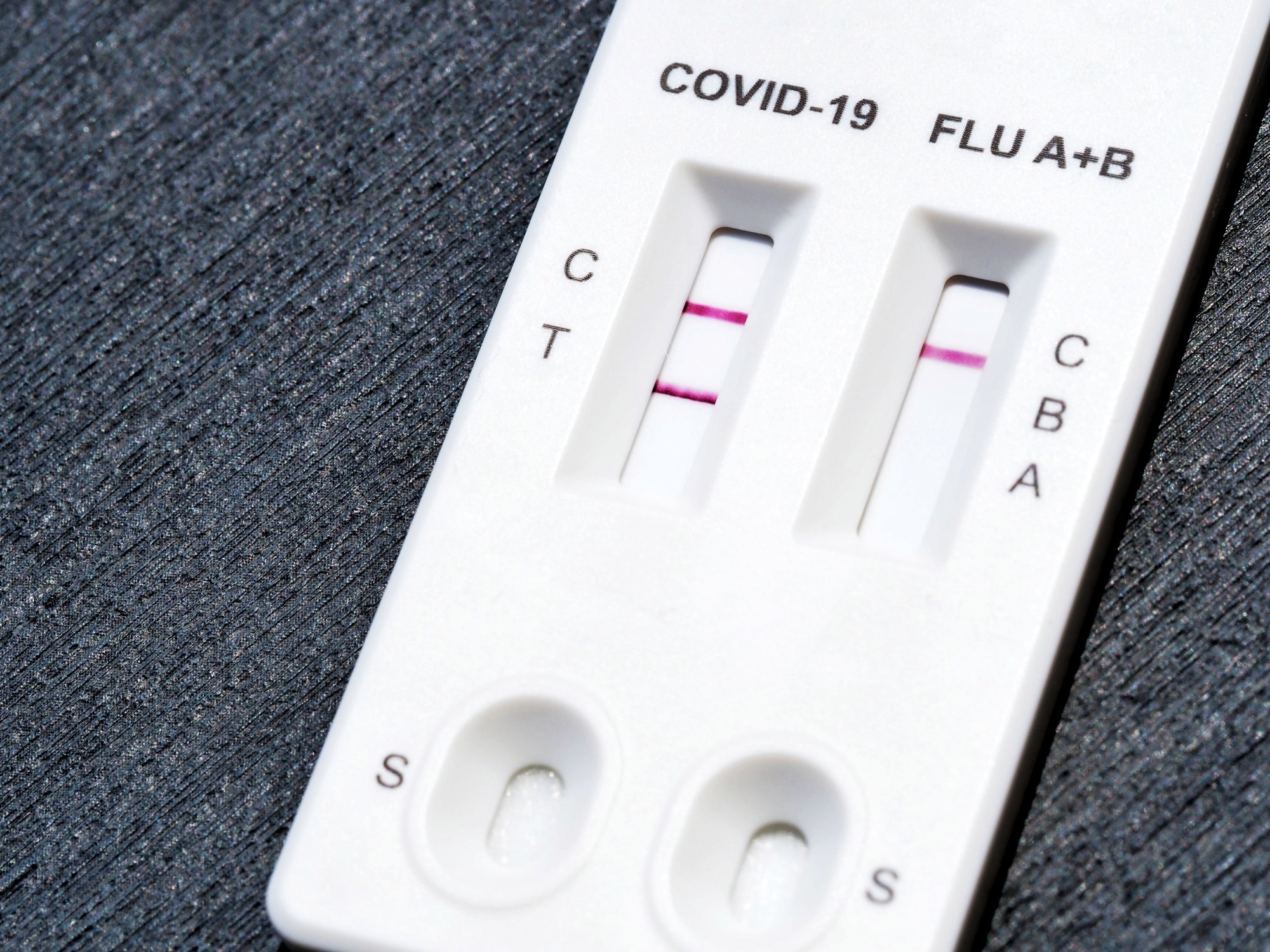 Study: Genetic risk factors for COVID-19 and influenza are largely distinct. PhotoRedHeart / Shutterstock
Study: Genetic risk factors for COVID-19 and influenza are largely distinct. PhotoRedHeart / Shutterstock
The study and findings
In the present study, researchers investigated whether COVID-19 and influenza have shared genetic etiology. First, a genome-wide association study (GWAS) of influenza was performed on data from more than 296,000 AncestryDNA COVID-19 study participants to explore how the same genetic factors influence the risk of influenza and COVID-19.
Of these, 6.2% reported having been influenza-positive and were classified cases. The remainder of the population served as controls, including approximately 24,000 with negative results. Next, the team assessed associations between 10 million common variants and reported influenza infection in three ancestral groups.
A meta-analysis of the results across ancestries identified two loci associated with reported influenza near β-1,3-galactosyltransferase 5 (B3GALT5) and ST6 β-galactoside α-2,6-sialyltransferase 1 (ST6GAL1) on chromosomes 3q27.3 and 21q22.2, respectively. Results from GWAS of influenza were used to evaluate whether influenza and SARS-CoV-2 infections share genetic etiology. To this end, they focused on 24 COVID-19-associated variants reported by the Host Genetics Initiative.
Only one variant, rs505922 in histo-blood group ABO system transferase (ABO), was associated with influenza; the variant reduced COVID-19 risk but increased the risk of influenza. The lack of directionally consistent and significant associations between influenza and COVID-19 loci suggested few or no shared genetic risk factors between the two diseases. Further analyses were performed to evaluate whether influenza associations were reproducible and robust.
Excluding over 253,800 people lacking data on influenza tests from the AncestryDNA cohort did not affect the effect size estimates for either locus. By contrast, defining influenza based on whether participants reported flu-like symptoms attenuated effect sizes, albeit they remained significant. In addition, to assess reproducibility, medical records were accessed to define the lifetime influenza status of 1.15 million participants from seven biobanks across five ancestries.
The researchers identified that only 2% were cases, whereas 1.13 million people (controls) lacked a lifetime influenza medical record. A meta-analysis revealed genome-wide significant and directionally consistent associations with B3GALT5 and ST6GAL1. Besides, two measures of recent influenza corroborated the associations. Significant associations were evident with a positive influenza A culture (indicating current infection) in a cohort of over 82,000 people.
Further, both variants reduced the risk of a seropositive influenza A test in a cohort of 1,000 people. Notably, the B3GALT5 variant reduced the risk of flu-related hospitalization among cases. No additional associations were identified. Moreover, no associations were observed between COVID-19 risk variants and influenza in this more extensive analysis. Next, the GWAS signal’s likely effector genes were identified, focusing on the lead variants at 3q27.3 and 21q22.2.
Four genes, adiponectin (ADIPOQ), immunoglobulin superfamily member 5 (IGSF5), B3GALT5, and ST6GAL1, were prioritized based on high linkage disequilibrium between each variant, and enhancer-overlapping variants and sentinel expression quantitative trait loci. Analysis of missense and loss-of-function variants (via exome sequencing) revealed no significant associations. However, a missense variant in IGSF5 was associated with a 9.2-fold increased risk of medical record influenza.
Finally, in vitro experiments were performed to examine the effects of gene expression knockdown on the infectivity of influenza H1N1 virus in Calu-3 and A549 cell lines, focusing on two likely effector genes: B3GALT5 and ST6GAL1. ST6GAL1 knockdown approximately reduced influenza infectivity by 50%, whereas B3GALT5 knockdown was not associated with a consistent effect on infectivity.
Conclusions
Taken together, the findings indicate that the genetic architectures of influenza and COVID-19 are largely distinct. The team identified genome-wide significant loci for influenza and showed that ST6GAL1 inhibition decreases infectivity in vitro. The study’s limitations include phenotype misclassification, use of self-reported influenza status, undetermined influenza strain, and confounding effects from unmeasured risk factors for influenza.