Their results indicate that mortality from coronavirus disease 2019 (COVID-19) is now the tenth leading cause of death in the U.S. and that across causes of death, the overall mortality rate is highest among African American or non-Hispanic Black individuals.
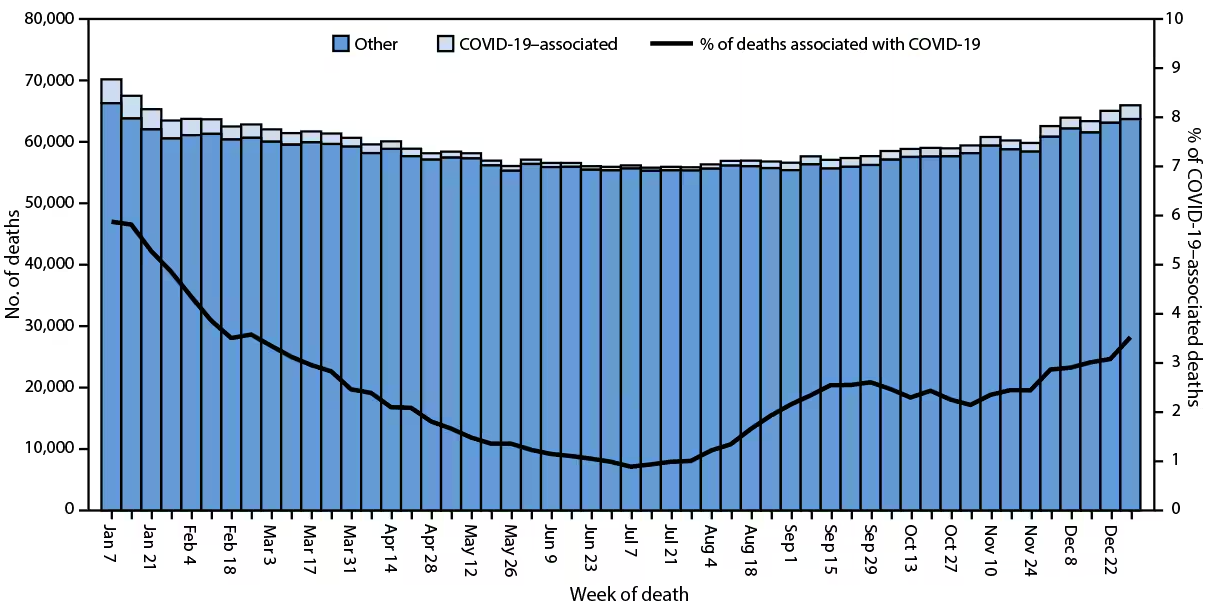
Provisional* number of COVID-19–associated deaths† and other deaths and percentage of deaths associated with COVID-19, by week of death — National Vital Statistics System, United States, 2023
Background
The National Center for Health Statistics (NCHS) collects and publishes yearly death statistics using data from certificates of death issued in the U.S. Final figures for each year are usually available 11 months later due to the time needed for thorough investigation and review.
However, provisional data, such as those used in this report, offer an early signal about shifts in mortality trends. These estimates help track changes in death trends and shape public health strategies aimed at reducing deaths, especially in high-mortality groups.
About the study
The National Vital Statistics System (NVSS) regularly releases provisional death data, including COVID-19 deaths. This report covers provisional data on mortality in the U.S. for 2023 and compares it to 2022. NCHS provided statistics on total deaths, including deaths attributed to COVID-19, breaking them down by race/ethnicity, age, and sex.
Researchers followed the International Classification of Diseases to identify the causes of mortality. Deaths with COVID-19 as a contributing or underlying cause were included in COVID-19 counts. They then ranked the most common causes of mortality based on these figures, excluding deaths abroad and in American territories.
Weekly death counts and rates were analyzed, with rates adjusted for age and calculated for overall deaths and by specific groups. Population estimates for these calculations came from the Census Bureau of the U.S.
Findings
In 2023, there were 3,090,582 deaths in the U.S., with an age-adjusted mortality rate of 750.4 for every 100,000 people, a 6.1% decrease from 2022. The highest death counts were in the weeks that ended January 7, during which time 68,965 died, and December 30, during which time 65,257 people died.
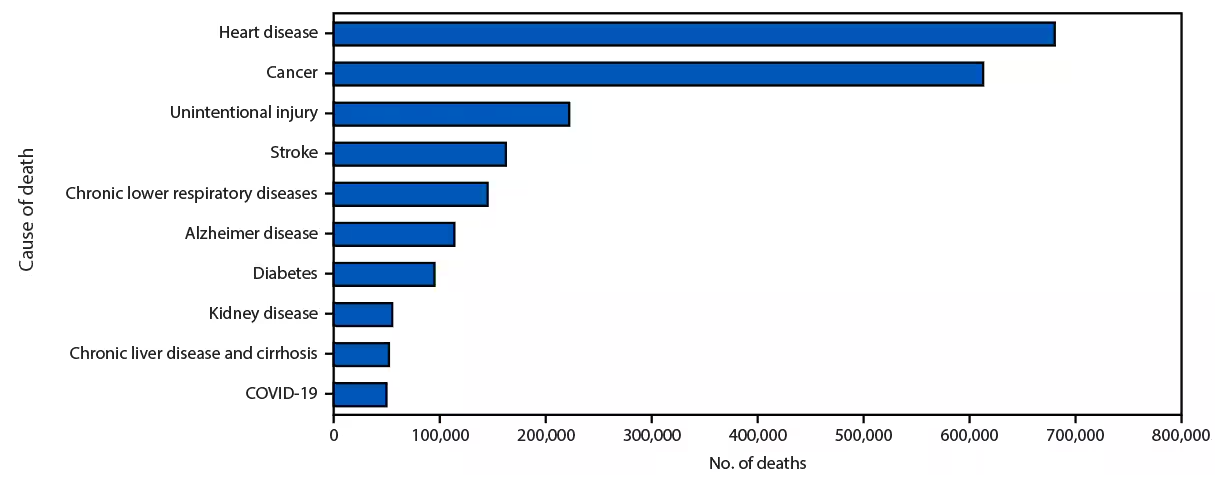
Leading underlying causes of death* — National Vital Statistics System, United States, 2023
People between the ages of 5 and 14 had the lowest death rate (14.7 per 100,000) and highest for those aged 85 and older (14,286 per 100,000). Death rates fell across every age group in 2023 compared to 2022, though not significantly among children aged up to four. The death rate adjusted for age was higher for males at 884.2 compared to females at 632.8, and both decreased from 2022.
Death rates varied by ethnicity and race, with multiracial individuals having the lowest rate (352.1 per 100,000) and Black individuals the highest (924.3 per 100,000). The most common causes of death included cancer, unintentional injuries, and heart disease. COVID-19, which was the fourth leading cause of death in 2022, became the 10th in 2023, accounting for 1.6% of deaths.
COVID-19 was implicated in 76,446 deaths in 2023, accounting for a death rate of 18.2 among every 100,000, representing a decrease of 68.9% from 2022. The death rate due to COVID-19 dropped across every age group and racial/ethnic group, with males (22.1 for every 100,000 individuals) having a higher rate than females, who had a death rate of 15.4 for every 100,000 individuals.
Conclusions
This report offers an initial overview of provisional mortality data for 2023, providing early insights into mortality trends. Such data are crucial for offering timely and actionable information, which can guide public health policies and interventions aimed at reducing mortality rates, particularly in populations experiencing higher mortality. These preliminary estimates are valuable for researchers and policymakers as they can signal shifts in mortality patterns sooner than final data.
However, the provisional nature of these data means they are subject to change. The estimates may be underrepresentative due to potential delays in death certificate submissions, which can vary by jurisdiction. Such delays, especially from jurisdictions with large populations, could skew the overall death rates and alter the national distribution of mortality data. Additionally, there is a risk of misclassification in racial and ethnic categories on death certificates, which could result in inaccuracies in reported death rates for some groups.
These limitations underscore the need for a cautious interpretation of the data and highlight the importance of final mortality figures for a more accurate and comprehensive understanding of mortality trends in the U.S.