Several months after recovering from coronavirus disease 2019 (COVID-19), patients with LC may continue to suffer from numerous symptoms, some of which include fatigue, brain fog, and chest pain. The prevalence of LC varies, with estimates ranging from 10-30% in non-hospitalized cases to 50-70% in hospitalized patients.
Although several digital health interventions (DHIs) and applications have been developed to monitor acute symptoms of COVID-19, few have been designed to track long-term symptoms of the disease. One DHI called "Living With COVID Recovery" (LWCR) was initiated to help individuals manage LC by self-reporting symptoms and tracking their intensity. However, there remains a lack of evidence on the risk factors, characteristics, and predictors of LC, thereby limiting the accurate identification of high-risk patients to target preventive strategies.
About the study
In the present study, researchers investigate the prevalence and intensity of self-reported LC symptoms to analyze their potential relationship with demographic factors to inform targeted interventions and management strategies. To this end, LWCR was used to monitor and analyze self-reported LC symptoms from individuals in 31 LC clinics throughout England and Wales.
The study included 1,008 participants who reported 1,604 unique symptoms. All patients provided informed consent for the use of their anonymized data for research.
Multiple linear regression analysis was used to explore the relationship between symptom intensity and factors such as time since registration, age, ethnicity, education, gender, and socioeconomic status through indices of multiple deprivation (IMD) on a scale of one to 10.
Education was classified into four levels denoted as NVQ 1-2, NVQ 3, NVQ 4, and NVQ 5, which reflected those who were least educated at A level, degree level, and postgraduate level, respectively. The intensity of symptoms was measured on a scale from zero to 10, with zero being the lowest and 10 the highest intensity. Descriptive statistics identified variations in symptom intensity across different demographic groups.
Study findings
Although 23% of patients experienced symptoms only once, 77% experienced symptoms multiple times. Corroborating with existing literature, the most prevalent symptoms included pain, neuropsychological issues, fatigue, and dyspnea, which affected 26.5%, 18.4%, 14.3%, and 7.4% of the cohort, respectively. Symptoms such as palpitations, light-headedness, insomnia, cough, diarrhea, and tinnitus were less prevalent.
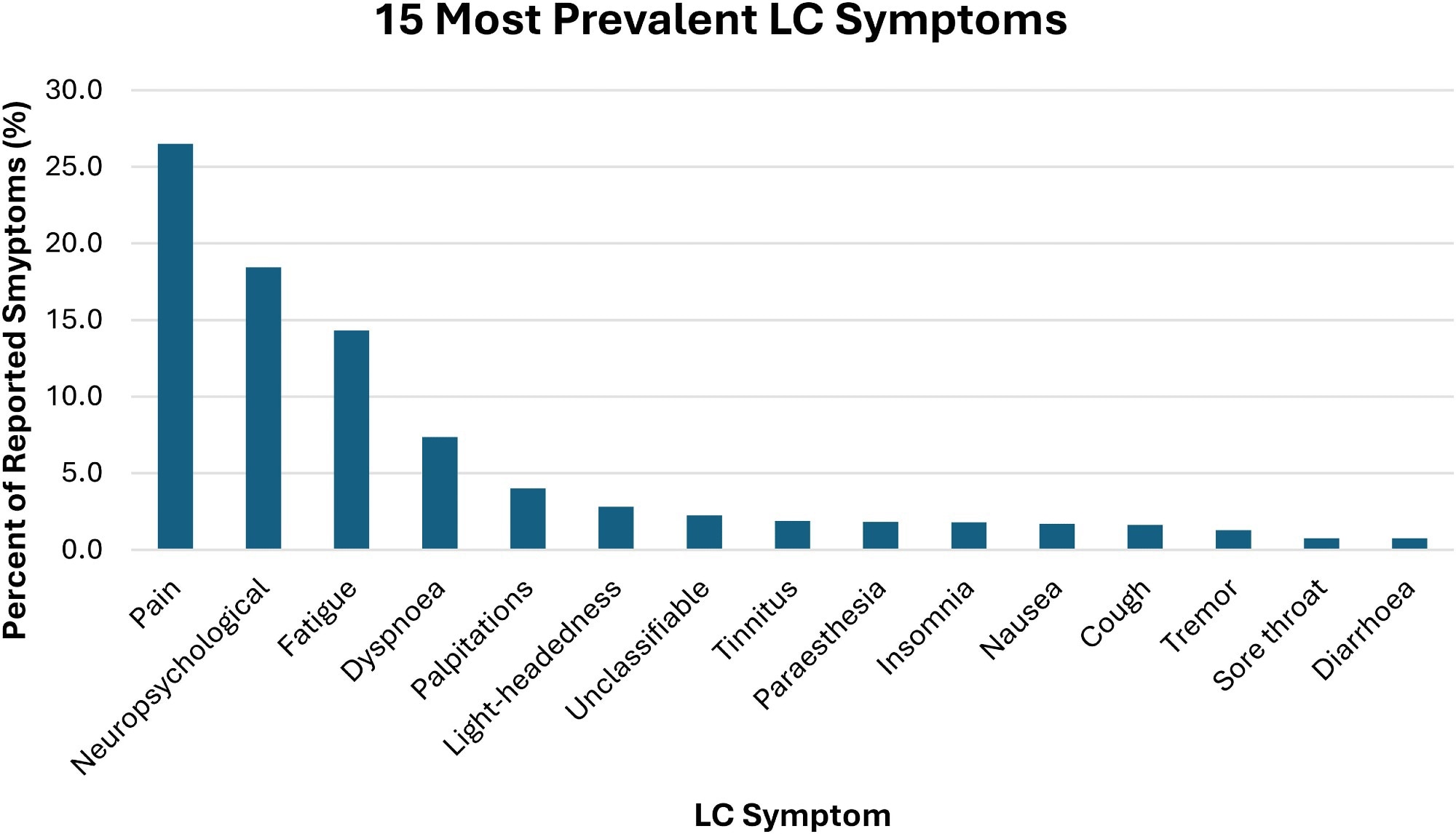 Fifteen most prevalent LC symptoms.
Fifteen most prevalent LC symptoms.
Multiple linear regression analysis revealed that symptom intensity was significantly associated with age, gender, ethnicity, education, and IMD decile. More specifically, individuals 68 years of age and older reported higher symptom intensity by 32.5% and 86%, respectively. These findings align with existing literature that highlights the increased risk of LC symptoms with age, which may be due to weakened immunity or the presence of comorbidities. Thus, they emphasize the need for targeted interventions for this population.
Females also reported higher symptom intensity than males, by 9.2%. Non-White individuals experienced higher symptom intensity by 23.5% as compared to White individuals.
Individuals with higher education levels reported up to 47% reduced symptom intensity as compared to those with lower education levels. Higher IMD deciles, which reflect less deprived areas, were associated with lower symptom intensity; however, no significant association was observed between the number of symptoms reported and the IMD decile.
A significant positive association was observed between symptom intensity and the duration between registration on the app and initial symptom reporting. This finding suggests individuals may become more aware of their symptoms or that worsening symptoms prompt reporting.
Some limitations of the current study include the lack of data on comorbidities, hospitalization, and vaccine status. There is also a potential for bias against individuals lacking technological proficiency or access, which may affect the sample's representativeness, particularly for older, socioeconomically disadvantaged, or non-English-speaking individuals. Excluding patients with severe symptoms or those who were ineligible for the app may also skew the findings.
Conclusions
There remains an urgent need to develop targeted interventions to address the severity of LC in relation to age, ethnicity, and socioeconomic factors. LC treatment should prioritize prevalent symptoms like pain, neuropsychological issues, fatigue, and dyspnea while also considering other possible symptoms. Furthermore, sustained support for LC clinics is essential to effectively manage the wide range of symptoms and complexities associated with LC and improve public health outcomes in the post-pandemic era.
Journal reference:
- Sunkersing, D., Goodfellow, H., Mu, Y., et al. (2024). Long COVID symptoms and demographic associations: A retrospective case series study using healthcare application data. JRSM Open 15(7). doi:10.1177/20542704241274292.