Background
Alcohol addiction is a global health issue linked to 5–8% of deaths worldwide and a higher risk of metabolic disorders. Long-term alcohol abuse is known to contribute to over 200 conditions, including various cancers. It impairs multiple organs, including the brain, endocrine, liver, heart, and digestive systems, while disrupting nutrient metabolism.
In the present review, researchers explored the effect of alcohol consumption on men's reproductive health and gonadal axis, focusing on the complex physiological and pathological mechanisms of alcohol metabolism and its interactions with other lifestyle factors, such as diet and physical activity.
Alcohol and Metabolic Health
Alcohol metabolism begins with absorption in the stomach and small intestine, followed by enzymatic processing in the liver through oxidative and non-oxidative pathways. In oxidative metabolism, enzymes like alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) convert alcohol into acetaldehyde and acetate, producing reactive oxygen species (ROS) and contributing to oxidative stress and inflammation.
Non-oxidative pathways generate metabolites such as fatty acid, ethyl esters, and phosphatidylethanol. Factors such as genetics, diet, comorbidities, and frequency and quantity of alcohol consumption influence individual metabolic efficiency.
Chronic alcohol consumption is linked to various diseases, including metabolic syndrome, type 2 diabetes (T2D), liver steatosis, and alcoholic liver diseases (ALD). ALD progression ranges from reversible fatty liver to severe conditions like alcoholic hepatitis, cirrhosis, and hepatocellular carcinoma.
Alcohol exacerbates insulin resistance, mitochondrial dysfunction, and oxidative stress, disrupting lipid metabolism and promoting inflammation. Interestingly, some studies suggest that light-to-moderate drinking may lower T2D risk, but heavy alcohol use increases liver damage and metabolic dysfunction through impaired insulin signaling, oxidative stress, and dysregulated cellular pathways.
Chronic alcohol intake leads to significant liver dysfunction through several mechanisms, including excess acetaldehyde production, oxidative stress, impaired lipid metabolism, and apoptosis.
Alcohol overconsumption disrupts gut microbiota balance and increases gut permeability, leading to elevated lipopolysaccharide (LPS) levels that activate immune cells and promote liver cell apoptosis, contributing to severe alcoholic hepatitis.
Recent evidence also suggests that alcohol-associated mitochondrial dysfunction exacerbates apoptosis and impairs hepatic regeneration.
Additionally, alcohol disrupts lipid and carbohydrate metabolism, impairing fatty acid oxidation, gluconeogenesis, and mitochondrial homeostasis, which results in liver fat accumulation and glucose intolerance. This metabolic dysregulation also promotes inflammatory cascades, oxidative damage, and epigenetic changes that may underlie alcohol-related metabolic syndrome.
 Multiple pathways involved in liver dysfunction under chronic alcohol consumption. ADH = alcohol dehydrogenase; AMPK = 5′ AMP-activated protein kinase; CYP2E1 = P450 2E1 cytochrome; DAMPs = damage-associated molecular patterns; cGAS-IRF3 = cyclic GMP–AMP synthase-interferon regulatory factor 3; PAMPs = gastrointestinal-derived pathogen-associated molecular patterns; PPARα = peroxisome proliferator-activated receptor alpha; LPS = lipopolysaccharide; ROS = reactive oxygen species.
Multiple pathways involved in liver dysfunction under chronic alcohol consumption. ADH = alcohol dehydrogenase; AMPK = 5′ AMP-activated protein kinase; CYP2E1 = P450 2E1 cytochrome; DAMPs = damage-associated molecular patterns; cGAS-IRF3 = cyclic GMP–AMP synthase-interferon regulatory factor 3; PAMPs = gastrointestinal-derived pathogen-associated molecular patterns; PPARα = peroxisome proliferator-activated receptor alpha; LPS = lipopolysaccharide; ROS = reactive oxygen species.
Alcohol’s Effect on Testosterone Production
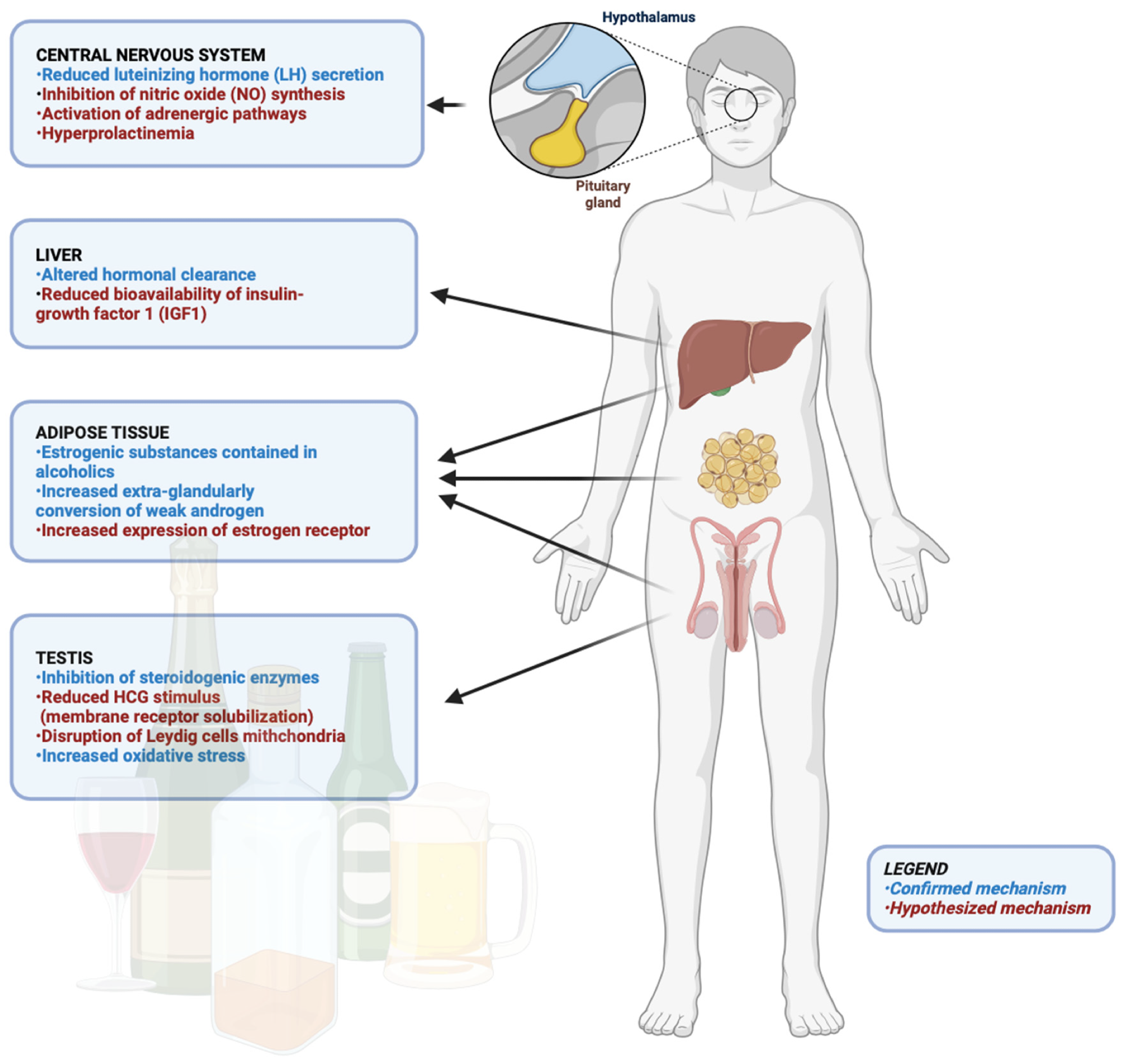
Alcohol consumption impacts testosterone production through complex mechanisms. Acute alcohol intake can lower testosterone levels by depleting NAD+, suppressing gonadotropins, and disrupting steroidogenesis while altering the hypothalamic-pituitary-gonadal (HPG) axis.
Chronic alcohol use typically reduces testosterone, with liver damage and hormonal imbalances (e.g., elevated estrogen) contributing. A meta-analysis noted that chronic alcohol consumption reduces serum testosterone by an average of 4.86 nmol/L compared to abstainers.
Alcohol abuse, especially binge drinking, often leads to feminization symptoms due to hyperestrogenism and oxidative stress-induced damage to Leydig cells. These effects vary with alcohol dose, liver health, and individual factors. Notably, the impacts of alcohol on testosterone production during adolescence, a critical developmental stage, remain underexplored and warrant further investigation.
Alcohol’s Effect on Male Reproductive Health
Alcohol consumption negatively affects male fertility, particularly through its impact on spermatogenesis. Acute alcohol intake may disrupt sperm production by elevating oxidative stress and impairing Sertoli cell function, although human studies show inconsistent results. Chronic alcohol use is more clearly linked to reduced semen quality, including lower sperm volume, concentration, and morphology.
Some evidence suggests moderate alcohol intake might have antioxidant benefits, but these findings remain inconclusive and context-dependent. Heavy alcohol abuse causes significant testicular damage, including spermatogenic arrest and Sertoli-cell-only syndrome. However, damage may be reversible with alcohol cessation.
A major limitation in research is the inability to account for confounding factors like smoking, drug use, and comorbidities, complicating conclusions about alcohol's effects on fertility.
Conclusion
In conclusion, the review highlights the negative effects of chronic alcohol consumption on metabolism and testicular function, including hormonal disruption, impaired spermatogenesis, and reduced sperm quality.
Additionally, alcohol abuse increases gut permeability and inflammation, triggering LPS and acetaldehyde-driven liver inflammation, mitochondrial dysfunction, and oxidative stress, which contribute to alcoholic fatty liver disease.
The findings could potentially inform public health strategies while emphasizing the importance of distinguishing between moderate, acute, and chronic alcohol use and the need for further research to guide clinical recommendations and preventive measures.