hMPV was first identified in 2001 and has been increasingly recognized as a respiratory pathogen with significant health implications. It is associated with various respiratory illnesses, such as lower and upper respiratory tract infections, and causes symptoms similar to other respiratory viruses. Therefore, the overlap in clinical findings between hMPV and other pathogens highlights the need for precise diagnostics.
hMPV mainly spreads via sneezing, coughing, close personal contact, and exposure to contaminated surfaces. These modes of transmission pose risks in healthcare settings, where proper control measures are essential to prevent nosocomial transmission. The virus remains transmissible for up to a week after symptom onset, as highlighted by the case report, necessitating vigilance among healthcare workers.
Severe manifestations are frequent in young children, older adults, and immunocompromised individuals. Studies on severe hMPV infection have primarily been on pediatric populations. As such, data on adult populations remain limited. CAP represents a significant cause of morbidity and mortality worldwide. Vaccination programs have successfully reduced bacterial CAP. Nonetheless, knowledge gaps persist regarding the microbial etiology of severe CAP requiring hospitalization, particularly for respiratory viruses like hMPV.
The Study and Findings
In the present study, researchers in Brazil described the case of severe pneumonia due to hMPV in an older, immunocompetent adult. The subject was a male aged 68 years with chronic aspirin use and a history of dyslipidemia and mild systemic arterial hypertension. The subject was physically active and non-smoker, without obesity, diabetes, or other comorbidities, and presented with progressively aggravating respiratory symptoms.
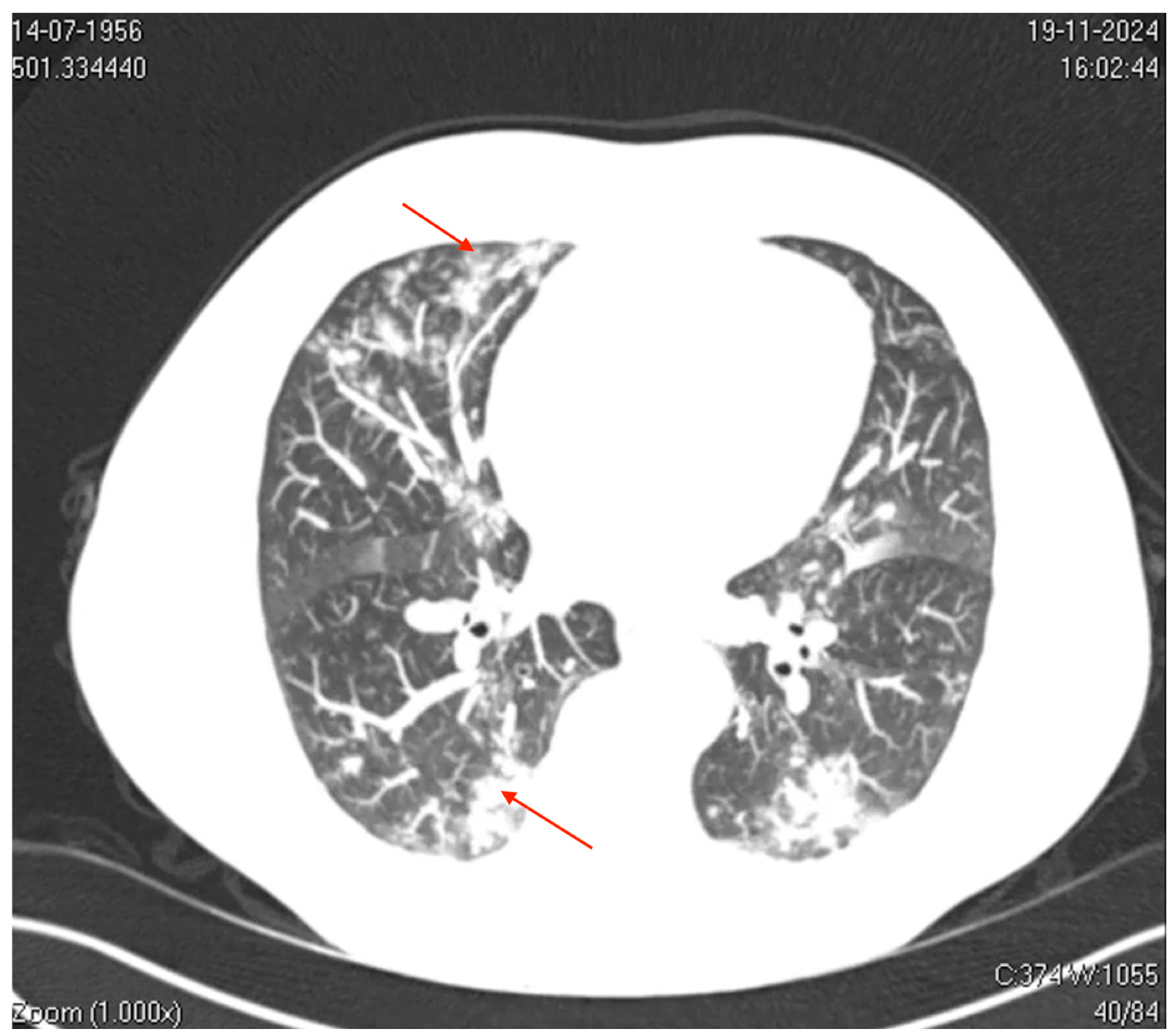
Axial computed tomography (CT) image of the thorax. The image shows bilateral ground-glass opacities with a reticular pattern interspersed with focal areas of consolidation and peripheral bronchiolar filling. The red arrows highlight specific areas of consolidation surrounded by ground-glass opacities, which are more prominent in the peripheral and lower lung regions. These findings suggest a diffuse inflammatory or infectious process involving the pulmonary interstitial and peripheral airways (acinus and bronchioles), which is consistent with viral pneumonia.
Initial symptoms (on day 1, D1) were intermittent dry cough and mild odynophagia, which progressed to nasal congestion, rhinorrhea, nocturnal sweating, and allodynia by D2. A self-administered nasopharyngeal swab test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was negative. Subsequently, the patient was started on amoxicillin-clavulanate, prednisone, and clarithromycin.
Nevertheless, the patient’s condition was exacerbated, with intense coughing, bronchospasm, myalgia, fatigue, and headache, prompting admission to the emergency department on D7. Laboratory findings revealed elevated inflammatory markers, including C-reactive protein (7.6 mg/dL) and D-dimer (870 ng/mL), thrombocytopenia, mild increase in transaminase, and normal procalcitonin and leucocyte levels, suggesting viral etiology. Imaging studies indicated significant pulmonary involvement.
Thoracic computed tomography (CT) showed mild bilateral pleural effusions, ground-glass opacities interspersed with areas of consolidation, and small centrilobular opacities. These findings were consistent with a viral pneumonia pattern and predominantly affected the left lower and upper lobes. Besides, CT of the paranasal sinuses revealed mucosal thickening in the frontal sinus.
During hospitalization, the subject received nebulization with oxygen, intravenous moxifloxacin, salbutamol, ipratropium bromide, and physiotherapy. The patient stabilized within 24 hours and was discharged on oral moxifloxacin. The subject improved gradually over the next week, achieving recovery by day 14 after discharge. During hospitalization, other diagnostic evaluations included molecular testing with a multiplex reverse-transcription polymerase chain reaction (RT-PCR) panel, which identified hMPV.
No other viral or bacterial pathogens were detected. Venous blood gas analysis indicated metabolic compensation, with a venous blood pH of 7.41 and bicarbonate levels of 30.4 mmol/L. Hematological findings revealed normal white blood cell levels, with neutrophilic predominance, and mild thrombocytopenia. Platelet levels stabilized the next day, and there were minimal fluctuations in hematological and inflammatory markers throughout the hospital stay.
Conclusions
The present study underscores that hMPV can cause significant pneumonia in immunocompetent adults with no comorbidities. This highlights the growing recognition of hMPV as a frequent cause of CAP in different age groups, especially with the decline of bacterial infections. Radiological findings, such as ground-glass opacities and bilateral consolidations, are characteristic of viral pneumonia, further supporting the diagnosis. Notably, despite molecular testing revealing hMPV as the sole pathogen, antibiotic therapy was started, reflecting persistent diagnostic uncertainty in differentiating bacterial and viral infections.
Overall, this case report emphasizes the importance of rapid molecular diagnostics for hMPV, enhancing management, and decreasing unnecessary antibiotic use. The study also highlights the global underdiagnosed burden of hMPV in adult populations, underscoring the need for its integration into routine diagnostic workflows. Integrating hMPV testing into routine clinical protocols could improve diagnosis and resource use. Moreover, addressing the global hMPV burden requires continued investment in diagnostics and therapies to ameliorate outcomes and reduce morbidity.
Additionally, vaccine development efforts, such as the investigational bivalent vaccine IVX-A12 targeting both hMPV and RSV, offer hope for reducing the disease burden and improving prevention strategies.
Journal reference:
Carmo, R., Saddy, F., Costa, J. L., Tavares, L. R., & Caire, H. (2024). The Silent Threat of Human Metapneumovirus: Clinical Challenges and Diagnostic Insights from a Severe Pneumonia Case. Microorganisms, 13(1), 73. DOI: 10.3390/microorganisms13010073, https://www.mdpi.com/2076-2607/13/1/73