Whether it is at school, nursery, or clubs, children spend much of their time away from home; it is, therefore, important that they always stay safe, especially if they suffer from asthma.
Adults who are responsible for children must be aware of what to do in the case of an asthma emergency.
Prevalence
Asthma is a common respiratory illness affecting roughly 5.4 million people in the UK—1.1 million are children.1,2 Asthma is the most common long-term illness among children and young people, and the UK has some of the highest mortality rates in Europe.
It is believed that emergency hospital admissions and fatalities related to asthma are largely preventable, with these statistics being correlated with poverty.2
Although there was a small decline in fatalities related to asthma among children and young people between 2008 and 2018, these figures are still too high for a condition that should be manageable, with more deaths avoidable.3
Regrettably, the trend seems to be increasing among young people aged between 15 and 24.3 Research from 2019 found that out of 19 countries, young people are more likely to die from asthma in the UK compared to other wealthy countries.4
Asthma and its symptoms
The British Thoracic Society and Scottish Intercollegiate Guidelines Network guidelines state that asthma can be defined as the occurrence of more than one of four symptoms: wheezing, coughing, breathlessness, and chest tightness.
Asthma is a combination of various inconsistent symptoms; sufferers may find that over weeks or months, they experience different symptoms. The underlying problem is the airways, which can have hyper-responsiveness (an increased sensitivity of the airways) or inflammation.
Asthma’s most common symptoms are wheezing, coughing, shortness of breath, exercise limitation, triggers, and duration of symptoms. These symptoms are variable and can come and go over time. The asthmatic person will often know what triggers their symptoms.
Asthma causes the mucous membrane to become inflamed, leading to swelling in the airspace, increased mucous production, bronchospasms, and twitchy airways.
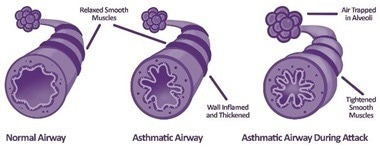
Image Credit: Bedfont® Scientific Ltd
Watch the webinar: Children with Asthma
Measuring asthma
There are several methods of measuring and monitoring asthma. One method is via a peak expiratory flow meter, a simple test in which a patient sets the scale on a metered device to zero, takes a deep breath, and then provides a short, sharp blow into the device.
Another technique is spirometry, a test that can be carried out in a clinic and offers a more sophisticated look at how air moves in and out of the chest. This test measures how much air someone can move out of their chest, how quickly this can be done, and the pattern the air follows as it leaves the chest.
Lastly, there is the fractional exhaled nitric oxide (FeNO) technique. Humans produce small amounts of NO in their breath, but when somebody has inflammation in the chest (often related to asthma), more NO is produced.
A FeNO test is carried out on the NObreath device and is suitable for people of all ages. It requires the patient to take a deep breath and blow out steadily into the device.

Image Credit: Bedfont® Scientific Ltd
Children and asthma
Asthma is a long-term, serious condition that can present physical symptoms if poorly controlled. These include shortness of breath, a tight chest, and wheezing in children.
These symptoms may lead to further issues in children: if they feel ill, they are less likely to exercise, which could then lead them to become deconditioned and at risk of obesity, which can make asthma even worse. Badly controlled asthma can disturb sleep, affecting children’s concentration, behavior, and emotions.
Badly controlled asthma can have many psychological effects on children. Asthma may make them feel different from their peers; they might also be embarrassed by their inhaler and may not use it when needed. The experience of asthma attacks in the past might also make them feel uncomfortable doing anything, which might trigger further attacks and may limit what they can do.
Bad control of asthma can also influence education outcomes, as children with asthma may be absent from school due to asthma attacks or attending medical appointments. Children might also have diminished concentration due to poor sleep or them feeling unwell.
Treating asthma
There are over a hundred different inhalers available and many options for treatment. The goal is for anyone with asthma to have no day or night symptoms, no limitations to activity, no need for a rescue inhaler, normal lung function, and no side effects from treatment.
The primary role of treating asthma involves treating the underlying inflammation, which leads to decreased swelling, the airways opening back up, and the patient finding it easier to breathe.

Image Credit: Bedfont® Scientific Ltd
Unfortunately, not all treatments are instantaneous; a brown-colored preventer inhaler must be used for at least a few days, allowing the medication to target the inflammation slowly. Once the inflammation has settled, the inhaler will likely be needed in the long term.
Inhalers can be divided into two categories: treatment and rescue. A treatment inhaler is a long-term treatment with no instant effect; it settles swelling and treats underlying inflammation. Rescue inhalers treat twitchy airways, relieve symptoms quickly, and last up to four hours for each use.

Image Credit: Bedfont® Scientific Ltd
Rescue inhalers should only be used occasionally; if someone uses one more than three times per week, it would suggest that their treatment is not quite right and should be assessed.
It is vital to know the difference between the inhalers: treatment inhalers are generally orange or brown in color, whereas rescue inhalers are always blue.
Maintenance and reliever therapy via a combination inhaler is also used. The combination inhaler contains rescue and treatment medication and is used twice daily if symptoms persist. Extra doses should only be required occasionally.
Getting the inhaler technique right is very important; unfortunately, sometimes, due to insufficient guidance from healthcare providers, many people do not know how to use their inhalers properly. Education is key when enabling patients to take medication correctly.
There are different types of inhalers:
- Pressurized metered-dose inhalers
- Breath-actuated metered-dose inhalers
- Spacer devices
- Dry powder inhalers
Knowing the different types of inhalers and how to use them is vital. For metered-dose inhalers, breathing should be slow and gentle; for dry powder inhalers, breathing should be fast and hard.
If the fast and hard breathing technique is used with a metered-dose inhaler, the medication will hit the throat rather than move to the lungs, and the reverse is true for dry powder inhalers.
Spacers (chambers for metered-dose inhalers that slow the speed of the medication and hold it for a few seconds, allowing the user more time to breathe it in) are available, usually for children. Depending on the users' age and capability, a range of spacer sizes is available.
Controlling asthma
Asthma can still flair up if all the previous steps are in place and a patient’s treatment is correct. To tackle this, patients should use treatment inhalers regularly, be aware of their triggers, know how to best use them, and attend regular reviews with asthma nurses.
Patients should make a GP appointment if the blue rescue inhaler is needed more than thrice weekly. If someone is short of breath and their blue inhaler is not helping, they should make a GP appointment for the same day.
Watch the webinar: Children with Asthma
Asthma attacks
Knowing what to do in the event of an asthma attack could be the difference between life and death. The below graphic from Asthma + Lung UK shows the steps to take during an attack.
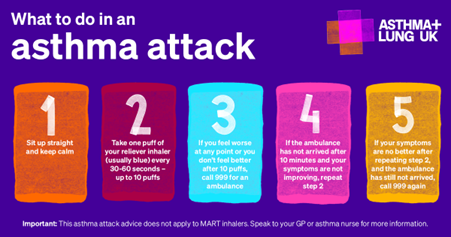
Image Credit: Asthma + Lung UK
Everyone should have a personalized asthma action plan to ensure the right treatment. Various formats are available; see below for an example from Asthma + Lung UK.
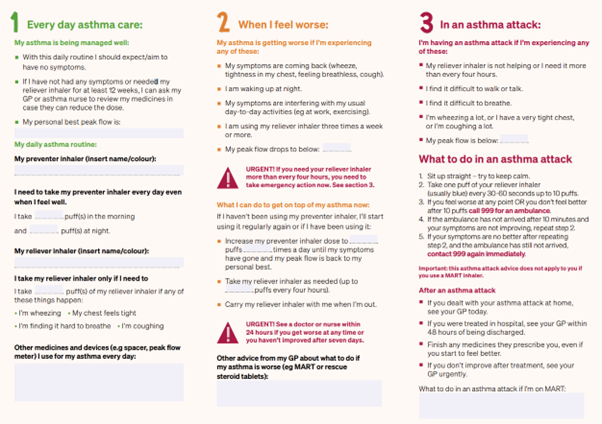
Image Credit: Asthma + Lung UK
The green area represents controlled asthma and the medication to maintain good control. The amber section refers to when things are worsening: how can asthma sufferers recognize when their condition is deteriorating? The section offers steps to improve symptoms and return to the green section.
The red area signifies an asthma emergency and what to do in these circumstances.
Asthma sufferers need to know when they are in the red section and what they need to do if this happens, but it is also helpful to realize when they are in the amber stage so they can get back into the green.
Seasons
Asthma is linked to the seasons, and there are times when we see peaks in hospital admissions: spring (pollen), autumn (back-to-school), and winter (winter colds).
The UK pollen calendar below shows peaks throughout the year.

Image Credit: Worcester University
Triggers
There are many asthma triggers, but the most common are exercise, chemical fumes, dust, smoke, pollution, strong odors, cold air, bugs in the home, fungus spores, anger, stress, and pets.
There are also some lesser-known triggers, including hormones, infection, changes in temperature, dampness and mold, thunderstorms, foods, alcohol, drugs, and sex.
Managing effects
Occasionally, triggers are unavoidable, but they should be eliminated or avoided where possible. Individuals should manage other conditions that trigger asthma and ensure it is managed well. Some triggers can be predicted: for example, if hay fever is a trigger, start treating this early. Asthma sufferers should always have their rescue medication in hand.
Parents and carers must understand asthma, know how the medication works, and why it is important. Responsible adults should make asthma action plans, know how to maintain control and know what to do in an emergency. They should also know what to do if an inhaler has been forgotten.
Want to know more? Click below to watch the full webinar
Watch the webinar: Children with Asthma
References and further reading
- Asthma + Lung UK (2021). What Is Asthma? [online] www.asthmaandlung.org.uk. Available at: https://www.asthmaandlung.org.uk/conditions/asthma/what-asthma.
- Royal College of Paediatrics and Child Health (2020). Asthma – RCPCH – State of Child Health. [online] stateofchildhealth.rcpch.ac.uk. Available at: https://stateofchildhealth.rcpch.ac.uk/evidence/long-term-conditions/asthma/.
- Chen, W.-Y., et al. (2021). Decreasing ten-year (2008–2018) trends of the prevalence of childhood asthma and air pollution in Southern Taiwan. World Allergy Organization Journal, [online] 14(5), p.100538. https://doi.org/10.1016/j.waojou.2021.100538.
- Asthma: Young people in the UK ‘more likely to die’. (2019). BBC News. [online] 20 Feb. Available at: https://www.bbc.co.uk/news/health-47292157.
About Bedfont® Scientific Ltd
Bedfont® Scientific has specialised in the design and manufacture of exhaled breath and gas monitoring instruments since 1976.
For medical gas monitoring, their Medi-Gas Check medical pipeline testing range verifies not only the quantity but also quality of gas administered to patients.
Bedfont's breath analysers include carbon monoxide (CO) monitors such as the Smokerlyzer®, used for smoking cessation, and the ToxCO®, used by emergency services, to diagnose CO poisoning.
The NObreath® FeNO monitor provides accurate analysis of airway inflammation for the control of asthma, and the Gastrolyzer® range aids in the detection of gastrointestinal disorders and food intolerances. Quick and non-invasive, breath analysis is the new blood test.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.