Skip to:
Osteoarthritis is a type of degenerative arthritis that most commonly affects joints in the hips, knees, lower back, neck, and fingers.

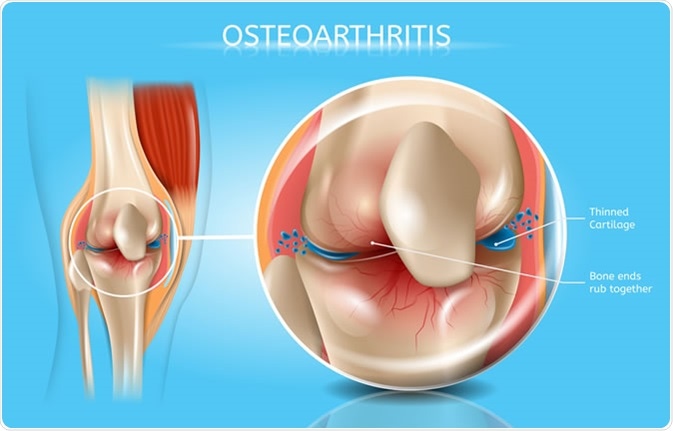
The model of knee joint shown the process of osteoarthritis of knee and total knee replacement surgery. Image Credit: Peter Porrini / Shutterstock
What is osteoarthritis?
Osteoarthritis (OA) is caused by breakdown of the cartilage that cover the bone ends and provide a cushioning effect between bones. Any damage to the cartilage can cause severe pain, swelling, and stiffness in joints, leading to movement difficulty.
If not managed properly, bones can be affected and spurs (small outgrowth of bone) can be developed gradually. Moreover, a local inflammation caused by OA can further damage the cartilage, making the condition more painful.
Although OA affects people at any age, it most commonly occurs after the age of 65 years. Women are more likely to develop OA than men. Other common risk factors include obesity, pre-existing joint injury, defective joints/cartilage, and overuse of joints.
Certain metabolic conditions, such as diabetes and hemochromatosis, also increase the chance of OA. In some rare cases, there is a genetic predisposition to OA.
What are the common complications of osteoarthritis?
Since OA is degenerative, the condition worsens gradually over time, leading to chronic joint pain. As a consequence, older patients with OA may face difficulty performing day-to-day activities. Moreover, an intensified pain, compromised mobility, and impaired balance can increase the chance of accidents and injuries.
People with OA are 30% more likely to experience falls. Moreover, they have a 20% higher risk of fracture.
In case of severe OA, a rapid and progressive loss of cartilage can occur (chondrolysis). Osteonecrosis or bone cell death is a serious complication that needs surgical intervention to remove the affected bone parts.
Osteoarthritis - Image Credit: TeraVector / Shutterstock
Since bones are exposed due to absence of the cartilage, repeated stress or injury to bones can result in hairline fractures. Some patients experience bleeding and infection inside and around joints, which further trigger the inflammatory processes.
Another common problem is loss of stability due to breakdown of tendons and ligaments around the affect joint.
Affected bones/cartilage may exert excessive pressure to a nerve, resulting in a pinched nerve. This damage interferes with normal functioning of the nerve, which further aggravates the pain and causes tingling, numbness or weakness.
The knee or hip joints OA can push a person toward a sedentary lifestyle, which can lead to weight gain and its associated risks of obesity, diabetes, cardiac complications, and cancers.
In knee OA, calcium crystals are sometimes deposited in the cartilage (chondrocalcinosis). Such crystals can flare-up OA symptoms and cause severe joint pain and swelling.
Another complication is cyst formation behind the knee. These cysts, commonly known as Baker’s cysts, put pressure on blood vessels and impair normal blood flow, leading to swelling and pain in the legs.
Chronic pain and disability may cause sleep deprivation in patients with OA. Over time, lack of sleep can cause undue emotional distress, including depression and anxiety.
The condition can also affect social life as well as family life, causing deterioration in overall quality of life.
Patients with OA who have high levels of uric acid in the blood are at higher risk of developing gout, which is a form of inflammatory arthritis.
Medicines, such as non-steroidal anti-inflammatory drugs, that are commonly used to treat OA can cause stomach upset, stomach bleeding, and ulcer.
Other adverse side-effects of these medicines include cardiovascular disorders (ischemia and myocardial infarction) and liver and kidney damage.
Living with osteoarthritis
Although there is no cure for OA, there are options to reduce the severity of the symptoms.
Exercise is the mainstay of treatment for OA and physical therapy may be helpful for patients to learn about the best exercises to maximize joint health and functionality.
Swimming, walking, low-intensity aerobic exercise, and stretching activities, are helpful for strengthening the muscles around the affected joint, improving joint flexibility, and reducing pain. A daily bout of physical activity is also helpful in managing body weight.
Assistive devices, such as canes, crutches, and walkers, can be used to avoid putting extra stress on the joints and improve stability.
Mild-to-moderate OA pain can also be managed with alternative therapies, including acupuncture, massage, relaxation methods, and hydrotherapy or with medications designed to reduce inflammation, which in turn reduces pain. Opioid medications should be avoided in chronic use and are best reserved for severe, short-term pain related to surgery or fracture.
If conventional treatment fails to manage OA symptoms, surgeries are performed to repair or replace the affected joint.
Further Reading
Last Updated: Dec 21, 2022