Neuroblastoma is a rare childhood cancer that develops from immature nerve cells called neuroblasts. “Neuro” means nerve, while “blast” refers to immature cells and “oma” means a tumor or group of cells. Neuroblastoma usually develops in infants under the age of five years and very rarely in older children, teenagers, and adults.
Neuroblastoma often arises in the abdomen, typically in and around the adrenal glands or the nerve tissue at the back of the abdomen. However, this cancer can also develop in other regions of the abdomen or in nerve tissue found in the neck, chest, spine, or pelvis.
In some cases, neuroblastoma can spread to areas other than the site of origin, most commonly the bone marrow, bones, liver, lymph nodes, and skin. This metastasis occurs in approximately 50% of children with the condition.
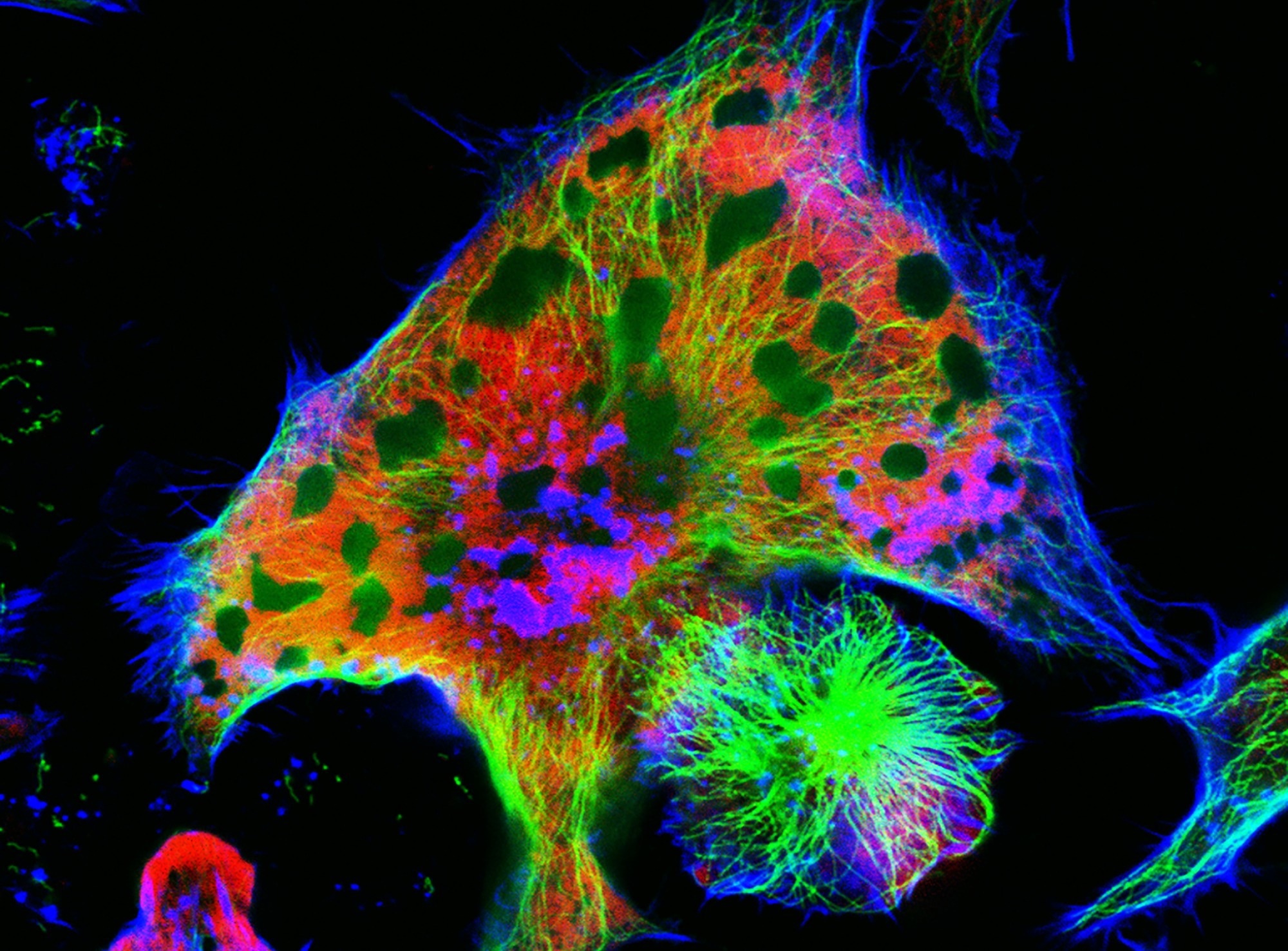
Image Credit: Vshivkova
Causes
In general, cancer arises due to a genetic mutation that enables healthy cells to continue growing when they would usually have responded to signals to stop growing. These cells then proliferate out of control and grow until they eventually form a mass or tumor.
As a fetus develops in the womb, neuroblasts eventually mature into fully formed nerve cells, nerve fibers, and the cells that form the adrenal glands. The majority of neuroblasts mature by birth, although a small proportion of immature neuroblasts may be present in newborns. Usually, these immature nerve cells develop into mature cells; however, in the case of neuroblastoma, they go on to form a tumor.
In cases where there is a family history of neuroblastoma, children are at an increased risk of developing the disease. However, familial neuroblastoma is only thought to account for a very small proportion of cases and, usually, the cause of the condition is not clear.
Chromosomal and molecular markers
Over the past several decades, researchers have identified several molecular and chromosomal abnormalities in patients with neuroblastoma. These abnormalities serve as biological markers of the condition and have been evaluated to establish their value in determining patient prognosis. Some of these markers are now used as part of risk assignment strategies.
The most significant of these markers is the oncogene MYCN, which has an official name of “v-myc avian myelocytomatosis viral oncogene neuroblastoma derived homolog.” This oncogene is overexpressed in around 25% of neuroblastoma cases and is believed to be due to amplification of the distal arm of chromosome 2.
The number of MYCN gene copies varies widely between neuroblastomas but is usually found to be between 50 and 100. Amplification of this gene is associated with a more aggressive form of this disease. Even in the presence of favorable factors such as low-stage disease, amplification of MYCN is associated with rapid cancer progression and a poor prognosis.
Prognosis
Important prognostic factors used for risk assessment and treatment decisions for patients with neuroblastoma are age, cancer stage, and the features of tumor cells.
Prognosis and treatment outcomes vary widely among these patients. Low-risk or intermediate-risk disease is often associated with an excellent prognosis and outcome, while the high-risk disease is associated with a very poor outcome, even when patients undergo intensive therapy.
Treatment Cures Boy’s Neuroblastoma, Leading To Cancer Breakthrough | Sunday TODAY
Unfortunately, among patients aged more than 18 months, around 75% present with metastatic cancer, typically in the bone marrow, bone, liver, and lymph nodes. Less than 50% of these patients are successfully treated, even when they are administered intensive therapy followed by autologous stem cell or bone marrow rescue.
References
- “Neuroblastoma.” Www.cancerresearchuk.org, www.nhs.uk/conditions/Neuroblastoma/Pages/Introduction.aspx http://www.nhs.uk/conditions/Neuroblastoma/Pages/Introduction.aspx
- www.cancer.org/acs/groups/cid/documents/webcontent/003125-pdf.pdf - Link no longer active
- Schell, Matthias, and Christophe Bergeron. Neuroblastoma. https://www.orpha.net/data/patho/GB/uk-neuroblastoma.pdf
- “Department of Pediatrics | the University of Chicago.” Pediatrics.uchicago.edu, pediatrics.uchicago.edu/. https://pediatrics.uchicago.edu/
- “Neuroblastoma.” Www.cancerresearchuk.org, www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/neuroblastoma.http://www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/neuroblastoma
- “Rare Cancers - Macmillan Cancer Support.” Www.macmillan.org.uk, www.macmillan.org.uk/Cancerinformation/Cancertypes/Childrenscancers/Typesofchildrenscancers/Neuroblastoma.aspx http://www.macmillan.org.uk/Cancerinformation/Cancertypes/Childrenscancers/Typesofchildrenscancers/Neuroblastoma.aspx
- “Neuroblastoma - Symptoms and Causes.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/neuroblastoma/basics/definition/con-20027487.http://www.mayoclinic.org/diseases-conditions/neuroblastoma/basics/definition/con-20027487
- “Pediatric Neuroblastoma: Practice Essentials, Pathophysiology, Etiology.” EMedicine, 18 Dec. 2023, emedicine.medscape.com/article/988284-overview. http://emedicine.medscape.com/article/988284-overview
Further Reading
Last Updated: Feb 20, 2024