T-cells are a critical component of the adaptive immune system and are indispensable in protecting humans from pathogenic infections. Changes in T-cell metabolism are a natural part of the immune response. However, downregulation of T-cell metabolism can lead to a reduction in the efficacy of T-cells against invading pathogens (known as immunodeficiency), leading to diseases such as cancer.
Skip to:
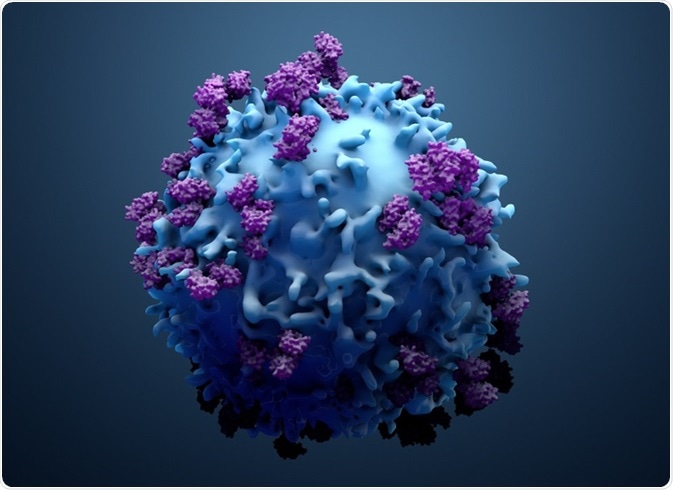 Design_Cells | Shutterstock
Design_Cells | Shutterstock
Metabolic responses of T-cells
The activation of a T cell causes epigenetic changes that can influence cell fate and metabolism. Changes in metabolism can provide substrates, like acetyl-CoA and methyl groups, which can further modify the activity of histone and DNA-modifying enzymes, exacerbating the effect. Metabolic changes can also influence the differentiation characteristics of T cells, a necessary step for an immune response – thus, the metabolic state can dictate susceptibility to certain diseases and also provide opportunities for therapeutic solutions.
T-cell metabolism and infectious diseases
Infection by microorganisms often leads to changes in the metabolism of the infected host. In acute infections, this may be accompanied by an increase in insulin resistance, protein catabolism, gluconeogenesis, and lipid metabolism. All of these changes can lead to hyperglycemia, amino acid abundance, and dyslipidemia.
CD4+ and CD8+ T-cells can initiate an immune response and induce the differentiation of effector populations. Such processes increase anabolic metabolism, ATP demands, and cell signaling events. On the other hand, reduction in the metabolic output due to inhibition can result in T-cell exhaustion, as is observed during chronic infection.
T-cell metabolism and quiescence
When the immune system has eliminated a pathogen, inflammatory responses and metabolic changes start to dissipate, leading to a reduction in the number of effector T-cells, followed by homeostasis and a metabolically quiescent stage.
During this period, memory T cells are produced, which protects the host cells from re-infection. The memory CD8+ T cell generation is supported by blocked glycolytic flux which suggests that metabolic stress on effector T cells potentiates the formation of memory cells.
Immunodeficiency
Primary immunodeficiencies are rare genetic diseases of the immune system that make the host susceptible to infection, resulting in autoimmune and immune dysregulation. Studies show that hypometabolic T cell-intrinsic state is associated with primary immunodeficiency. In this case, the patients have reduced basal and activation-induced glycolysis and capacity for oxidative phosphorylation.
Metabolic syndromes
Overnutrition and obesity-related signals can lead to increased inflammation and disrupted metabolic homeostasis. Metabolic syndromes are associated with various risk factors, such as obesity, hyperglycemia, dyslipidemia, and high blood pressure. Immune cells, like T-cells, are able to detect the availability of nutrients, leading to altered immune cell activation and inflammation.
The response of immune cells to these signals can reduce insulin signaling in tissues that have an active metabolism, thus promoting insulin resistance and type 2 diabetes. Studies show that changes in lipid content, such as saturated fatty acids and polyunsaturated fatty acids, can actually change the state of effector T cells from inflammatory to regulatory.
Autoimmunity
Studies have shown that an increase in glucose uptake by T-cells can stimulate the production of interferon and interleukin-2, leading to stimulation and deposition of antibodies in the glomeruli of the kidney.
The increase in the glucose uptake was brought about by overexpression of GLUT1 in T cells. Similarly, deletion of Glut1 leads to reduced uptake of glucose and reduced number of CD4+T cell generation. Therefore, glucose metabolism of T cell can influence the autoimmune status.
T-cell metabolism and cancer
Within a tumor, immune cells are often actively competing with the cancer cells for nutritional resources. This is due to a limited amount of glucose, amino acids, fatty acids, and similarities in the metabolic program of malignant cell expansion and expansion of CD8+ effector T cells. Finally, studies reveal that the subtype of T cells are dependent on various metabolic modules for their survival and for their anticancer effector functions.
Further Reading
Last Updated: May 13, 2019