IPF (Idiopathic Pulmonary Fibrosis) is a difficult disease to diagnose. Many patients will experience many visits to the doctor and some may even be told they have a different respiratory condition before they finally get the correct diagnosis that they do have IPF. In some patients the whole process can take more than a year.
However the moment when a patient finally receives an accurate diagnosis of IPF can be confusing and overwhelming. It is a devastating disease, and because it’s a rare condition many patients may not have heard of it or know what it means to have IPF. That’s why sharing a diagnosis of IPF with a patient can be one of the hardest things we have to do.
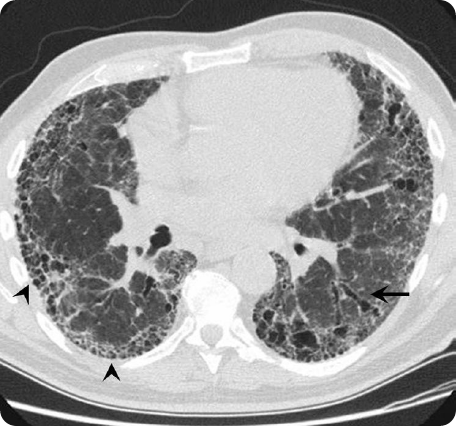
HRCT scan of an IPF patient. Adapted from Meltzer & Noble Orphanet Journal of Rare Diseases 2008.
Can you please give an overview of the recent global survey of IPF patients that asked questions on their diagnosis discussion? What were the main aims behind this survey?
The results of the global survey, supported by Boehringer Ingelheim, of over 120 patients, give us a real understanding of the information needs and priorities of patients when they’ve been told they have IPF. These results complement a 2015 Boehringer Ingelheim global survey of over 400 pulmonologists.
Together the results allow us to compare physician and patients’ priorities; examine how aligned they are and ultimately help to identify gaps in understanding.
More results from the patient survey are also expected over the next year, providing further insights into the reality of living with this condition.
What were the main findings and were you surprised by the feedback?
An unexpected, but positive finding is that 9 out of 10 patients were happy with the way in which they were informed of their IPF diagnosis, an encouraging finding as it suggests physicians are communicating in a way patients appreciate.
That high number may also suggest that in addition to doctors communicating well, finally the patients know what they actually have and can now discuss the future and their therapy plan with their physician.
What additional information would patients like to receive at the time of diagnosis?
The survey found that in a group of patients 60% want to know what other support is available to them to help them live with IPF.
For example, they often want to know about support available through their general practitioner. They also want to know where to go to get advice and support from other people who are living with the condition; and this is where patient groups play such an important role.
After diagnosis, patients will now know that they have a condition where their lung function and ability to breath will decline, so they want to know what treatment options are available and which will be most appropriate for them.
Additionally, as IPF is such a little known condition, many patients want to know the facts about what the future holds as well as the realities of living with IPF over the longer term.
How could this be implemented?
It is important for physicians to continue to be aware of patient needs, and tailor the information they provide to these needs. Specialist nurses can also play an important role in identifying specific needs, providing information and supporting patients.
Physicians can also put patients in touch with national and international patient groups such as the European Idiopathic Pulmonary Fibrosis and Related Disorders Federation (EU-IPFF), who can play a crucial role in providing information, including emotional support and practical tips on how to best live with IPF.
When patients are stressed and anxious they can forget or misunderstand parts of a diagnosis discussion. What advice do you have for patients in this situation?
It is common that patients may only remember half or less of what was talked about in the consultation. So inviting a partner, family member or friend to appointments can also help the patient remember what is said on the day, as well as provide them the emotional support they may need after diagnosis.
It’s also important that patients tell their physician if they have any questions or if there is something that they have not understood. This will help physicians provide relevant information that will meet their specific needs.
Making lists with the questions you wish to ask may be one of the practical solutions to optimize the consultation with the physician.
What can healthcare professionals do to make sure patients have understood the diagnosis and can recall the necessary information?
When any patient is told they have cancer they can relate to this diagnosis and understand the impact of it, however when a patient is told they have IPF there is usually a big question mark for the patient and their friends or family, it’s a lot to take in.
Therefore, providing clear and careful information delivered in a caring way is needed from physicians.
But also pacing information, checking if patients understand and repeating some aspects in follow-up consultations may help to improve understanding.
What are patients’ top priorities after IPF diagnosis?
One of the top priorities seen in the survey is that patients want to see an expert in the field such as a pulmonologist who specialises in IPF. This makes sense because if you have a rare disease you want to deal with an expert who is familiar with your condition and treating patients with IPF.
Another priority is information because IPF and everything about it is likely to be new to them, so patients want to know about the disease. They also want to know about treatment options, new developments and if these are appropriate for them.
Encouragingly, these results closely matched with the results of the pulmonologist survey showing that physicians have a good understanding of patient priorities at this time.
What more can be done to improve the discussion further?
It is reassuring that the survey shows that a good understanding exists between patients and physicians at time of diagnosis, but there is still more that may be done.
Needs will change throughout the course of the disease and reassessment and discussion on these should be a continuous integrated part of care.
Where can readers find more information?
There are some great resources online about IPF, for example patient recourses like:
- Life with IPF website
- Boehringer Ingelheim has recently launched a new patient e-Book,
Endorsed by the EU-IPFF. It describes the IPF patient journey and provides further helpful resources.
The e-Book can be downloaded for free on iTunes store (apple.co/2cLuw0a) and Google play (https://bit.ly/2czw8Zi).
About Dr. Marlies Wijsenbeek
 Marlies Wijsenbeek is a pulmonary physician at the Erasmus MC University Medical Centre in Rotterdam, a national expert centre for interstitial lung diseases (ILD) in the Netherlands.
Marlies Wijsenbeek is a pulmonary physician at the Erasmus MC University Medical Centre in Rotterdam, a national expert centre for interstitial lung diseases (ILD) in the Netherlands.
Dr Wijsenbeek is chair of the multidisciplinary ILD centre and deputy head of the department of pulmonary medicine.
Her research interests include patient centred outcome measures in ILD, cough in IPF and new therapies in IPF and sarcoidosis.
Dr Wijsenbeek is secretary of the Dutch National ILD section and member of the (scientific) advisory board of the European Idiopathic Pulmonary Fibrosis & Related Disorders Federation, Dutch Sarcoidosis Patient Association and the Dutch Pulmonary Fibrosis Patient Association.