Researchers from the University of Pennsylvania's Abramson Cancer Center have developed two experimental immunotherapy methods that include one chimeric antigen receptor (CAR) T cell therapy for the treatment of multiple myeloma patients who were not responding to other treatments.
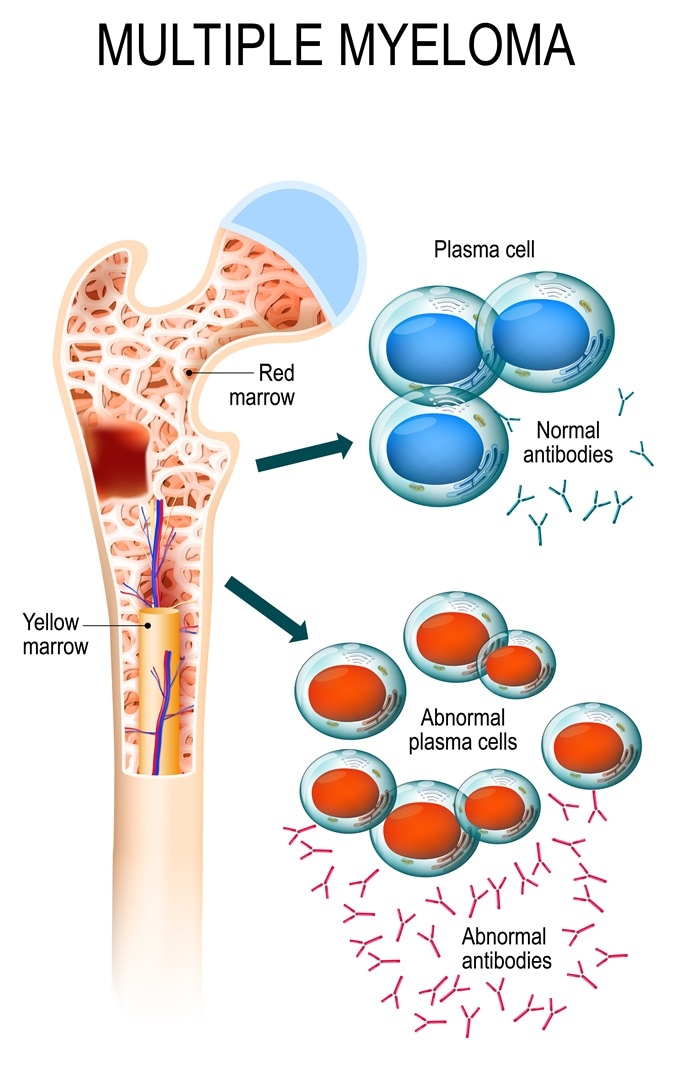
Multiple myeloma is a cancer of the bone marrow. healthy plasma cells in the bone marrow mutate and multiply uncontrollably. malignant plasma cells produce a paraprotein. Image Credit: Designua / Shutterstock
The other study used a monoclonal antibody in treatment of multiple myeloma. Both of the studies would be presented as oral abstracts at the 59th Annual American Society of Hematology Meeting and Exposition in Atlanta.
The team of researchers administered CAR T cells to the multiple myeloma patients after they had undergone chemotherapy and found that 64 percent of the patients responded favorably after the therapy. In the other study an experimental monoclonal antibody was infused into patients with resistant multiple myeloma and an overall response rate of 60 percent was noted. According to the researchers that receptor targeted in both these immunotherapy approaches is called the B-Cell Maturation Antigen (BCMA). BCMA occurs in high abundance in patients with myeloma and thus can be used as a target for these drugs in multiple myeloma.
Multiple myeloma affects thousands of patients every year. According to the American Cancer Society the estimated number of new cases this year is around 30,200 and these patients are usually treated with chemotherapy, radiation therapy and stem cell transplant. Multiple myeloma affects particular immune cells called the plasma cells that become cancerous and multiply uncontrollably.
Study 1
The first study is presented as Abstract #505 which involves the use of CART-BCMA. Here the CAR T cells are developed specially by the researchers in collaboration with Novartis over the past five years. Patient’s own immune cells are collected and they are modified in such a manner so that they can find and destroy the cancer cells specifically. These are termed “hunter” cells that can target the BCMA receptor that is present over the cancer cells and can multiply within the body to kill the cancer cells. The normal white blood cells are suppressed first using a chemotherapy cycle before infusing these CAR-T cells. The patients included in the experimental clinical trial had all failed with traditional treatment before being enrolled for the study. On an average they had received some seven lines of therapy before this study and failed to respond adequately.
The group was divided into two dose groups of the CART-BCMA therapy – the lower dose included 5 patients and the higher dosage group had 10 patients. The lower dosage group showed minor response in at least 2 patients. Minor response was defined as 25 percent or more reduction in the levels of myeloma protein. In the higher dosage group, minor response was seen in eight patients (80 percent) and one patient showed complete response. The clinical trial is not yet concluded and more patients are being treated with the higher dose level. Of the 15 patients, side effects such as cytokine-release syndrome which manifests as flu like syndrome, nausea, fever, muscle pain etc. was noted in 12 patients. For this side effect one patient received tocilizumab and another received siltuximab as therapy. No deaths were seen during the study and three patients developed some nerve toxicity that did not persist. Study’s lead author Adam D. Cohen, assistant professor of Hematology and Oncology at Penn and the director of Myeloma Immunotherapy in Penn's Abramson Cancer Center emphasized the importance of BCMA as an important target in treating multiple myeloma. The study was supported by the Penn-Novartis alliance.
Study 2
The second study presented as Abstract #741 used an experimental drug called GSK2857916. Dr. Cohen led this study as well. This new experimental drug was given breakthrough therapy designation by the US FDA this November so that it could be developed in an expedited fashion. This drug is combination of a chemotherapy drug called MMAF and a monoclonal antibody that targets the BCMA.
For the trial, 35 patients were given 16 treatment cycles with this experimental drug every three weeks. At the end of the study, 21 out of 35 (60 percent) showed some response to the drug. Around 51 percent showed a good partial response which meant that their myeloma protein levels reduced by over 90 percent. Media time that the patient spent without the disease progressing was around eight months.
Significant side effects in this study included eye toxicities such as dry eyes and blurry vision that was seen in 63 percent patients. Cohen added that there was a high response rate which had never been seen among these cases which were unresponsive to routine treatments.