Researchers have confirmed the existence of progenitor cells in the pancreas that can be stimulated to turn into glucose-responsive beta cells, a finding that could lead to the development of regenerative cell therapies for type 1 diabetes.
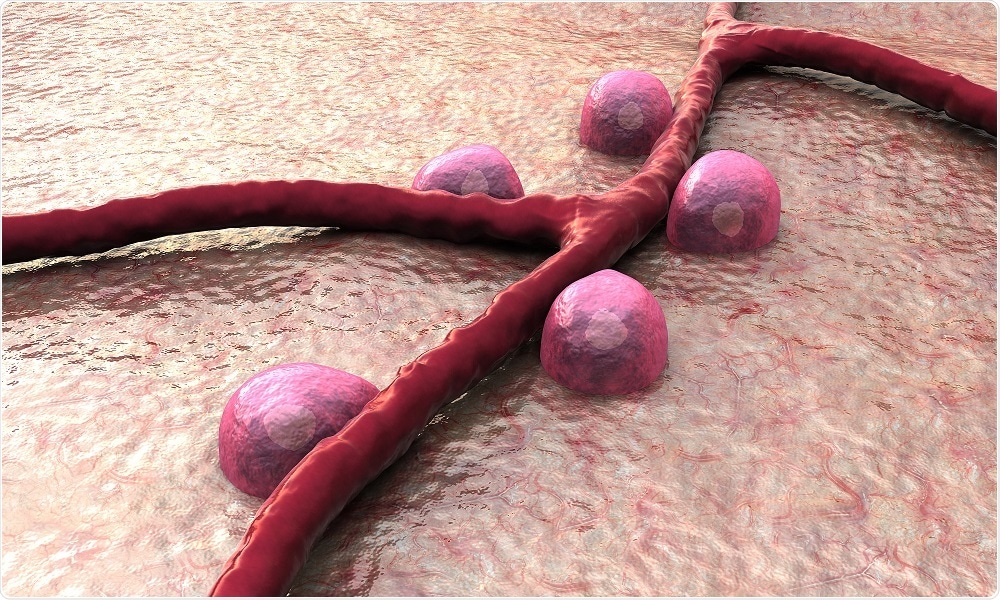 Credit: URGREEN 3S/Shutterstock.com
Credit: URGREEN 3S/Shutterstock.com
The possibility that the pancreas harbors progenitor cells that could regenerate islets has been suggested for decades, but has never been proven, until now. A new study has located those stem cells, and confirmed their ability to develop into glucose-responsive beta cells.
Our in-depth study of these pancreatic stem cells may help us tap into an endogenous cell supply 'bank' for beta cell regeneration purposes and, in the future, lead to therapeutic applications for people living with type 1 diabetes."
Dr. Juan Dominguez-Bendala, Co-Author and Researcher at The Diabetes Research Institute at the University of Miami
Dominguez-Bendala and team have previously shown that a growth factor called bone morphogenetic protein 7 (BMP-7) stimulates progenitor-like cells within cultured human non-endocrine pancreatic tissue.
In the current study, they have shown that those stem cells exist in the ductal and glandular network of the pancreas. In addition, the cells express PDX1, a protein that is required for the development of beta cells. They also express a cell surface receptor called ALK3 that has been associated with tissue regeneration.
Using “molecular fishing” techniques the researchers were able to extract the cells that express these two proteins, culture them and show that the presence of BMP-7 triggered their proliferation and differentiation into beta cells.
"Together with our previous findings using BMP-7 to stimulate their growth, we believe that we may be able to induce these stem cells to become functional islets," said Dominguez-Bendala.
It is hoped that the findings will aid in the development of regenerative cell therapies for the treatment of both type 1 and type 2 diabetes.
In type 1 diabetes, this would require abrogation of autoimmunity to avoid immune destruction of the newly formed insulin producing cells. For this reason our current efforts are converging on immune tolerance induction without the need for life long anti-rejection drugs."
Camillo Ricordi, Director of the Diabetes Research Institute, The University of Miami