May 9 2018
New research published in The Journal of Physiology has indicated a potential new stem cell treatment following a heart attack, by encouraging the regeneration of heart muscle cells. The low retention and survival rate of stem cells implanted in the heart had previously proven a sticking point for stem cell therapy following a heart attack.
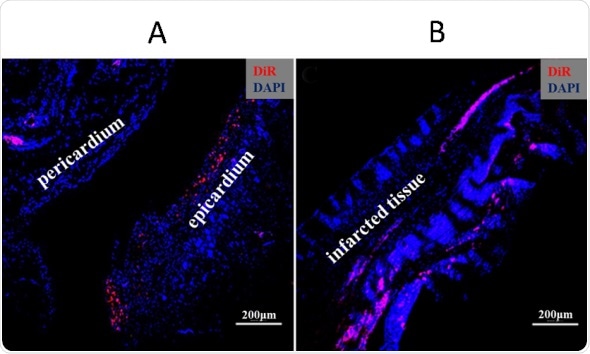
Immunofluorescence of cardiac tissue below, courtesy of Dr J Zhang:
A) Red-labeled (DiR) cardiospheres survived in the pericardium and infiltrated into the epicardium (the outer layer of the cardiac muscle wall – the myocardium) four weeks after the intrapericardial implantation; the areas of cells in both pericardium and myocardium are blue-labeled (DAPI, nucleus labeling).
B) Red-labeled cardiospheres migrated into infarcted myocardial tissue four weeks after implantation.
Stem cells are unspecialized cells which can become specialized cell types (e.g. cells in heart muscles). The research team used a new form of stem cell clusters derived outside of the body from the native stem cells of heart tissue, called cardiospheres. A cardiosphere’s structure comprises of non-specialised stem cells in the core, and more specialized heart cells on the outer layer. This structure mimics the native environment of stem cells in the heart muscle, and has been shown to lead to a better stem cell survival rate compared to conventional methods of implantation. They are therefore able to make up the cell loss in the heart following a heart attack. However, delivering these stem cell clusters to patients by conventional routes is difficult, due to the risk of them entering blood circulation and blocking blood vessels (an embolism).
Intrapericardial administration is the delivery of medicine into the pericardium, a double-layered sac around the heart. It has received little attention as a delivery route for stem cells, yet is commonly used for drug delivery to treat heart disease. As such, the researchers decided upon an intrapericardial method to deliver the cardiospheres, in the belief that the pericardial cavity would retain them, prevent micro-embolization and limit the loss of stem cells into other tissue or circulation. These cardiospheres were ‘optimised’ by a pre-treatment with a fluid from the pericardial cavity before being delivered through the pericardium in rats in an experimental model of heart attack.
After four weeks’ time, analyses were performed on the heart tissue. Results showed increased survival and retention rate of the implanted stem cells in the heart. In addition, there was higher migration of stem cells from the pericardium to the heart muscle, including the area affected by the heart attack. There was much improved heart function and survival rate compared to previous methods under comparable conditions. These findings suggest intrapericardial implantation is a promising delivery route for stem cell therapy in clinical applications, and that stem cell viability and function can be enhanced outside of the body prior to implantation, resulting in improved regeneration of heart muscle following heart attack.
Despite the promising results yielded by this study, it is important to note that this study may have been limited due to the fact the data obtained were from rats, and thus extrapolation of the findings to humans necessitates caution. As it is the first investigation on the application of pre-optimised cardiospheres via a pericardial route to treat heart attack, further studies will be required to clarify certain questions, including how implanted stem cells migrate from the pericardial cavity into the heart muscle tissue, and which specific molecules enhance stem cell potency outside of the body and promote cell regeneration in the heart muscle.
Changhao Wu, one of the research investigators, commented on the significance of the results:
This research could lead to new treatments for people after suffering a heart attack, as it shows how we can promote the regeneration of cells in the heart. The migration of the implanted stem cells from pericardium into the area of the heart affected by heart attack is an important finding. We were very excited as this result showed that implanted stem cells can directly differentiate into heart muscle cells. The membranes separating the pericardium and tissue in the heart muscle have tightly packed cells to limit cell penetration. Therefore, one would imagine that it would be difficult for the stem cells to migrate.