Researchers from Mount Sinai School of Medicine have discovered a new gene that is associated with disease severity in rheumatoid arthritis. It is hoped that the finding will lead to new treatments and new ways of assessing the prognosis of patients with the condition.
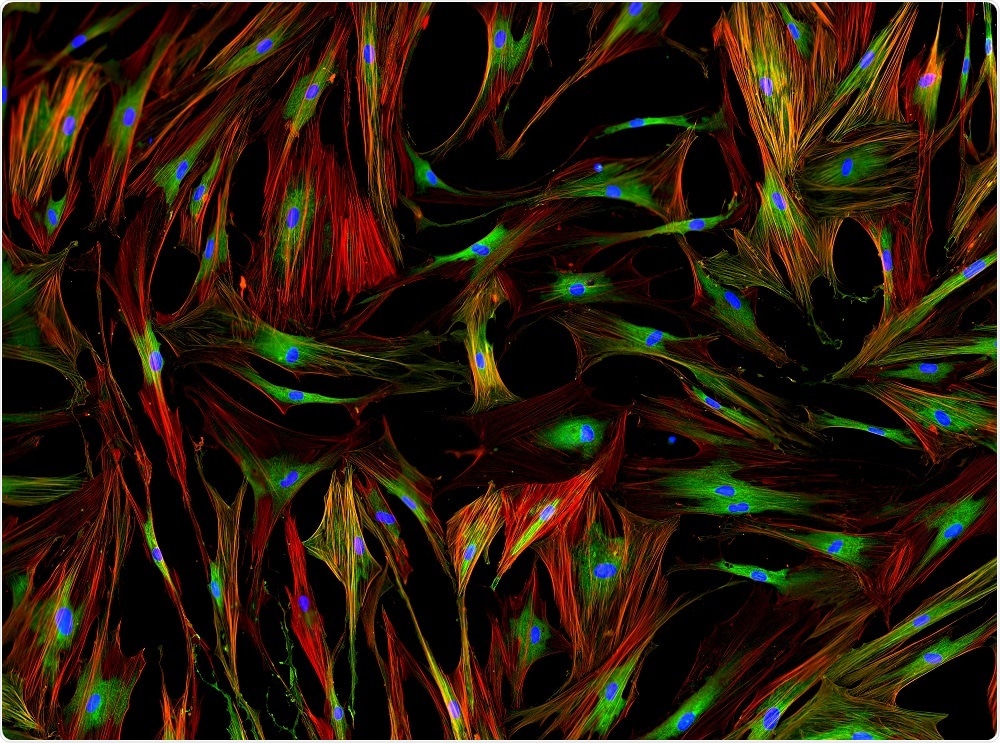 Image Credit: Damian Ryszawy / Shutterstock
Image Credit: Damian Ryszawy / Shutterstock
As reported in Annals of the Rheumatic Diseases, Percio Gulko and colleagues have shown for the first time that the gene HIP1 is a driver of inflammatory arthritis severity and cell invasiveness.
Current treatments for this autoimmune condition target the body’s immune response, but they are associated with a risk of immunosuppression and increased vulnerability to infection.
At my laboratory, we have been looking for alternative strategies. In this research, we have focused on understanding the regulation of disease severity and joint damage. Our discovery led us to the synovial fibroblasts, cells inside the joint.
Percio Gulko, Senior Author
Synovial fibroblasts produce components of the synovial fluid that lubricates joints and nourishes the cartilage.
In rheumatoid arthritis, the number of these fibroblasts is elevated and they become invasive. Immune cells then infiltrate the synovial tissue, which causes swelling and pain in the joint.
In the study, Gulko and team used genetic approaches including linkage mapping and congenic breeding, where certain fragments of chromosomes in arthritis-susceptible rodent strains are replaced with fragments from disease-resistant strains.
This led the researchers to a chromosomal region, made up of 41 genes, that drives arthritis severity and joint damage.
Upon sequencing this region, they identified a mutation in HIP1 that affected the behaviour of synovial fibroblasts. HIP1 has never previously been shown to have any association with inflammation or arthritis.
Next, the team took synovial fibroblasts from rheumatoid arthritis patients and knocked out the HIP1 gene, which significantly reduced the ability of the fibroblasts to respond to platelet-derived growth factor (PDGF).
PDGF induces the invasiveness of synovial fibroblasts and its expression is increased in the joints of patients with rheumatoid arthritis.
The researchers also studied mice that were deficient in HIP1 and found that they developed a milder form of arthritis. The team now plans to test the effectiveness of a therapy that will target HIP1.
We are aiming for a novel way of treating the disease. One that targets the synovial fibroblast, while sparing the immune system outside the joint.”
Percio Gulko, Senior Author
Source:
https://www.eurekalert.org/pub_releases/2018-07/tmsh-rin072418.php