 Image Credit: Meletios Verras / Shutterstock
Image Credit: Meletios Verras / Shutterstock
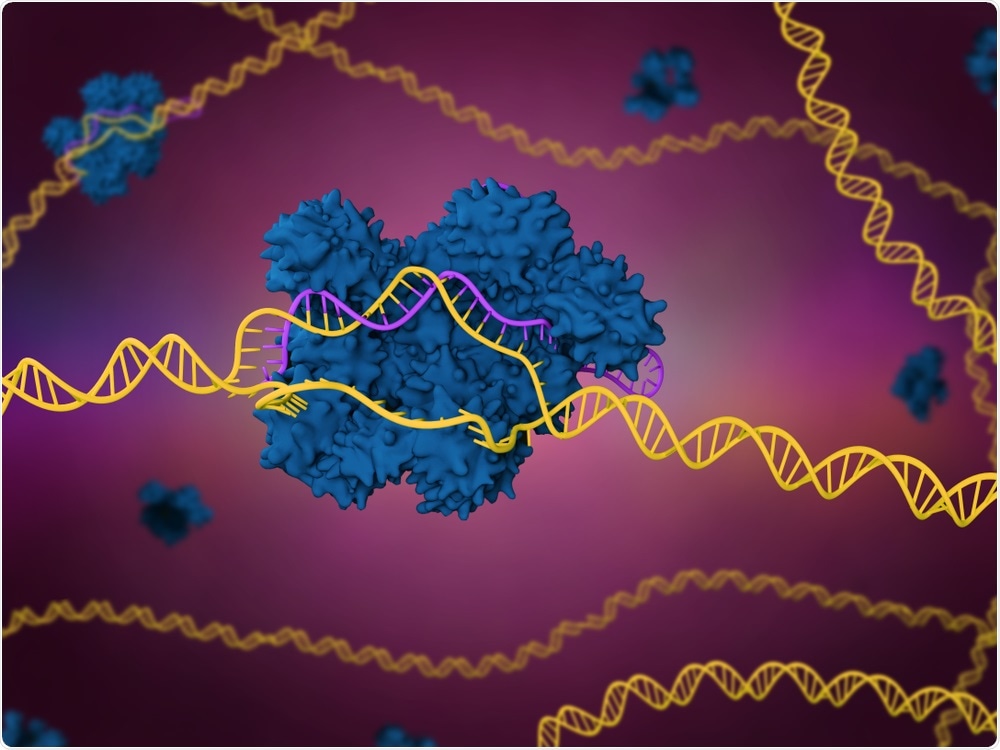
In a mouse model, the researchers used CRISPR-Cas9 and base editor 3 (BE3) gene-editing tools to target a gene that controls cholesterol levels and reduce cholesterol in utero.
Using prenatal gene editing, they also improved liver function and prevented neonatal death in mice engineered to have a mutation that causes a fatal liver disease.
In humans, this disease, which is called hereditary tyrosinemia type 1 (HT1), typically appears during infancy and can be treated with a drug called nitisinone and by following a certain diet.
However, in cases where treatment fails, patients can develop liver failure or liver cancer.
A prenatal treatment approach could pave the way for the prevention of not only HT1, but other congenital conditions.
Our ultimate goal is to translate the approach used in these proof-of-concept studies to treat severe diseases diagnosed early in pregnancy.
We hope to broaden this strategy to intervene prenatally in congenital diseases that currently have no effective treatment for most patients, and result in death or severe complications in infants."
Dr. William Peranteau, Co-author
For the study, the researchers used base editing to switch off the effects of a disease-causing mutation, but they plan to use the same technique to correct the mutation directly.
The BE3 tool is potentially safer to use than CRISPR-Cas9 since it does not completely cut the DNA and make it susceptible to unanticipated errors as the cut is repaired.
In this study, the team used BE3 to create a partially active CRISPR-Cas9 tool that specifically targets genes in the liver cells of mice in utero.
Following birth, the edited liver cells remained stable for up to three months, with no evidence of off-target editing of the DNA.
In mice engineered to have HT1, liver function and survival were improved. The mice were also healthier than mice that were administered nitisinone.
Peranteau says a significant amount of work is still needed before prenatal gene editing can be translated to the clinic, including studies into more clinically relevant delivery mechanisms and the safety of the approach.
Nonetheless, we are excited about the potential of this approach to treat genetic diseases of the liver and other organs for which few therapeutic options exist.