A warning from the U.S Food and Drug Administration (FDA) was issued yesterday after a patient died due to receiving a fecal transplant that contained drug-resistant bacteria. Such transplants are carried out to treat the infection Clostridium difficile (C. difficile) in patients who have failed to respond to standard treatments.
 Kateryna Kon | Shutterstock
Kateryna Kon | Shutterstock
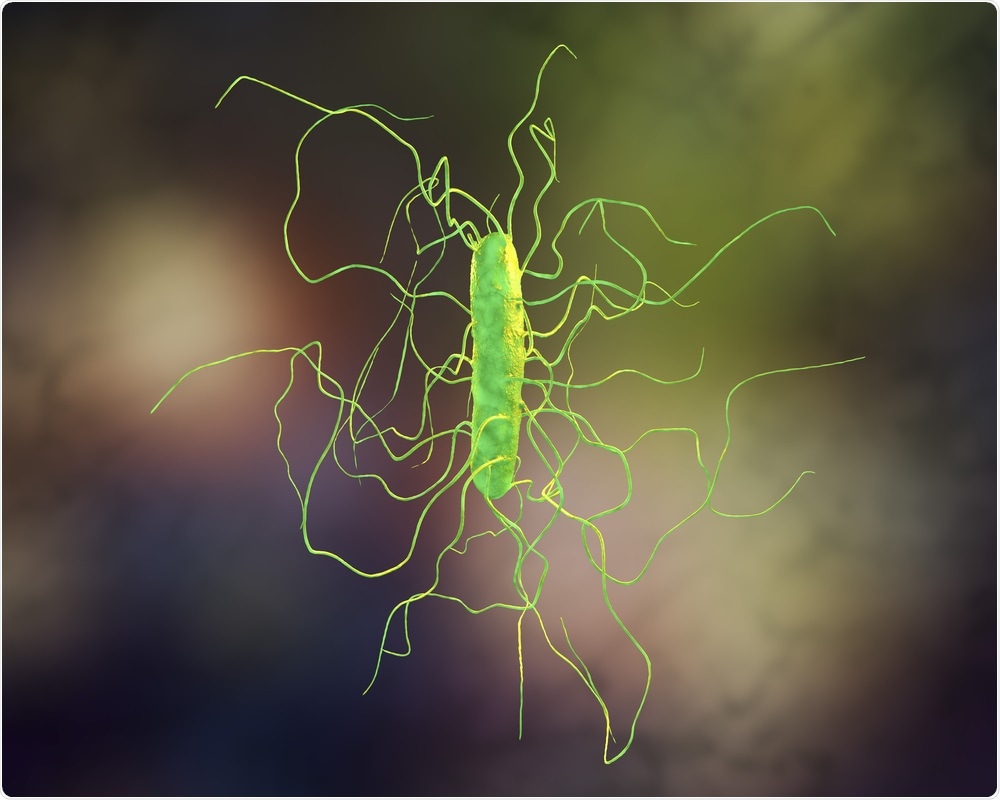
Recurrent C. difficile infections are caused by overgrowth of the microbe, which occurs when the normal composition of the gut microbiome becomes disrupted (dysbiosis) by the administration of antibiotics. Typically, the treatment approach is the use of long-term antibiotics. However, recurrence is common and the infection can be debilitating and lead to significantly reduced quality of life and poor health.
Fecal transplants provide an alternative to antibiotics
A fecal transplant involves slightly processed feces from a healthy person being transferred to the infected person’s gut to introduce beneficial or “friendly” bacteria. The procedure is intended to restore a diverse and stable gut microbiome that is in keeping with what would be considered a healthy bowel.
A fecal transplant provides a more favorable combination of microbial species and strains that complements and replaces a microbiome that has become imbalanced. This restores stability, with the resulting microbiome comprised of all the necessary microorganisms.
The only currently approved application of fecal transfer is in the treatment of recurrent C.difficile that continues after standard antibiotic treatment has been used. When the fecal transplant is used, relapse rates are significantly reduced.
How do fecal transplants help patients overcome C. difficile infections?
The gut microbiota is become increasingly important to researchers who have been discovering more and more about how it functions and contributes to bodily health.
A disturbed gut microbiome can contribute to a number of chronic gut disorders and metabolic conditions such as diabetes and obesity. In this context, fecal transfer has emerged as promising approach to restoring a healthy gut microbiome in order to treat diseases of the gut. Evidence has previously demonstrated absolute efficacy when the approach is used to treat recurrent C. difficile.
However, there are still questions surrounding the issues of safety and best practice. As interest in the benefits of fecal transplant grows, the potential need for better regulation is being brought to the fore.
The FDA report
The FDA reports that two adult patients with compromised immune systems who had transplants from the same donor became heavily infected with Escherichia coli (E.coli) that produces enzymes called extended-spectrum beta-lactamase (ESBL).
Bacteria that produce ESBLs are resistant to many antibiotics including penicillin and cephalosporin. The ESBLs most commonly produced by E.coli are called CTX-M enzymes. When E.coli produces ESBLs, urinary tract infections develop that can lead to more serious infections such as septicemia, which can be fatal.
When E.coli produces ESBLs and is therefore resistant to drugs, the infection becomes much more difficult to treat.
The FDA says the stool was not checked for the presence of drug-resistant bacteria before the procedure. This only happened once the patients became ill, when a stored sample was tested and found to contain the resistant E.coli that had infected both patients.
The failing in procedure has triggered the FDA to state that all potential donors must be screened from now on with questions and stool tests for drug-resistant bacteria.
According to the Centers for Disease Control and Prevention (CDC), C. difficile causes almost half a million illnesses annually and can affect all age groups. The CDC also refers to antibiotic resistance as one of the largest public health threats we face today.
One report by the CDC found that in the U.S., at least two million individuals acquire drug-resistant infections, which results in death in at least 23,000 cases.