A new study published in the journal Nature Communications on 22 October 2019 reports a new approach to cancer treatment that increases the immune capability of T lymphocytes against malignant cancers. This allows the T cells to successfully infiltrate and destroy these tumors. Animal trials have been completed and the researchers are planning clinical trials in human beings next.
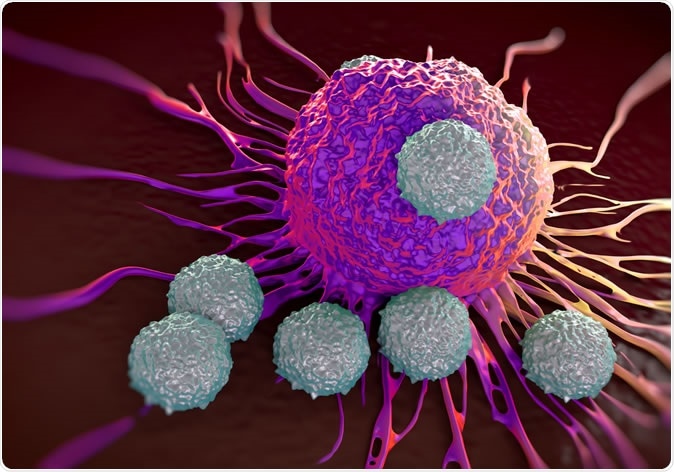
T-cells attacking cancer cell illustration of microscopic photos. Image Credit: royaltystockphoto.com / Shutterstock
What is immunotherapy?
Immunotherapy has been the start of a new age of cancer treatments, including immune checkpoint blockade against inhibitory receptors like PD-1 (programmed cell death-1), to increase T cell responses. T cells are the lymphocyte subset directly involved in cellular attack on foreign cells and particles, including malignant cells. Another mechanism that has been exploited is the direct suppression of signaling pathways that reduce T cell responses to tumor-related neoantigens. Both these pathways result in T cell activation, which is accompanied by regulators that prevent excessive inflammation and autoimmunity due to hyperactive T cell responses.
The study – Rasal1
The present study takes note of the role of a T cell molecule called Rasal1 (Ras protein activator-like 1 protein) that appears after T cell activation. This molecule binds to the T cell receptor (TCR) complex that is responsible for initiating all T cell responses to foreign antigens. The effect of Rasal1 binding to the TCR is to inhibit further activation pathways within the T cells, causing T cell anergy or unresponsiveness towards cancer antigens.
Two pathways of T cell inhibition via Rasal1
The experiments showed that T cell activation by the binding of anti-CD3 antibodies to the TCR led to an increase in both Rasal1 at 24 hours and 48 hours, in both CD4 and CD8+ cells. The anti-CD3 antibodies caused the Rasal1 to move from the cytoplasm to the membranes of the activated T cells. It then associates with the ZAP-70 which is a protein kinase enzyme linked to T cell activation, and suppresses its activity, causing inhibition of T cell activity.
This molecule also acts on extracellular-activated kinase (ERK) of the Ras–Raf-MEK-ERK pathway that activates T cells. Overall, the Rasal1 binding to the TCR causes reduced proliferative activity of T cells in proportion to the degree of receptor binding by the antigen. When the expression of Rasal1 within the T cells is reduced, T cells proliferate more actively and also have a higher cell expansion capacity.
Limiting tumor growth via Rasal1 downregulation
These findings were confirmed in a mouse model. When T cells with low levels of Rasal1 activity were transferred into mice with metastatic melanoma in the lung, the tumor’s growth was slowed. This was associated with a threefold increase in the number of T cells with CD8+ antigens on the cell surface. The tumor-infiltrating lymphocytes from these mice also showed a greater number of CD8+ cells with granzyme B and interferon γ-1 (IFN-γ1), two molecules that are responsible for cancer cell destruction by cytotoxic T cells.
When T cells with low Rasal1 levels were injected into another mouse model, this time with a solid lymphoma, tumor size reduced significantly from a mean of 570 mg to 370 mg, while the number of infiltrating T cells in the tumor increased fourfold, indicating a robust immune attack on the tumor cells. Molecular markers that signpost T cell activation were also increased, along with the effector molecules granzyme B and IFN-γ1. Thus T cell proliferation and activation level was increased by suppressing the expression of Rasal1, along with a slowing of the growth of the solid tumor.
Conclusion and implications
The current study picked up a novel T cell pathway that could help increase the effectiveness of cancer immunotherapy. This pathway involves the molecule Rasal1, which is shown to reduce T cell activity against cancer cells. Rasal1 seems to be only weakly present in inactive T cells and may therefore be upregulated only after the initial activation of T cells, to prevent inappropriate immune responses which could damage the host.
The inhibitory effect of Rasal1 on T cell activation was found to occur both in the cell cultures and in animal models. It occurs via two main pathways, one involving the ZAP-70 protein and the other via the p21-ERK pathway. On the other hand, T cells that do not express Rasal1 actively reduced the growth rate of metastatic lung melanomas solid lymphomas in mouse models.
T cells without Rasal1 expression have a greater anti-tumor effect. This is associated with a significant rise in the number of tumor-infiltrating T cells with the CD8 antigen. There is also an accompanying marked rise in the expression of killer effector molecules granzyme B (GZMB) and IFN-γ1, which directly kill tumor cells. This makes it potentially useful in cancer immunotherapy by inhibiting Rasal1, or to develop specific T cells that have higher anti-tumor immunity via already established approaches like CART.
Researcher Christopher E. Rudd says, “Hyperactivation of T cells enables them to penetrate and attack tumors. This discovery demonstrates that modulation of the identified [T cell] protein can activate the immune system and lead to destruction of the cancer cells.”
Source:
Journal reference:
GTPase-activating protein Rasal1 associates with ZAP-70 of the TCR and negatively regulates T-cell tumor immunity. Youg Raj Thaker, Monika Raab, Klaus Strebhardt & Christopher E. Rudd. Nature Communications 10, Article number: 4804 (2019). https://doi.org/10.1038/s41467-019-12544-4. https://www.nature.com/articles/s41467-019-12544-4#article-info