The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been rapidly spreading all over the world, affecting over 1.27 million people and killing almost 70,000 to date. Millions more are at risk. The chances of dying of this illness are as high as 11%, 7%, and 6% in patients with CVD, diabetes, and hypertension.
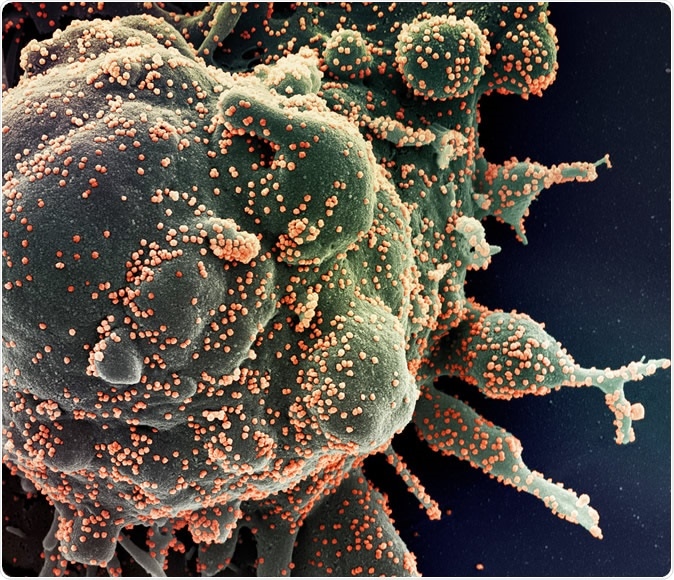
Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (orange), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
One class of medications that is used extensively in these patients is the renin-angiotensin system (RAS) blocker class. These include the angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs). The viewpoint includes information on the mechanisms of action, which may contribute to the usefulness of these drugs, the current guidance on their use in COVID-19 patients, and future research areas.
The virus and the receptor
The virus causing COVID-19 binds to a cell surface receptor called the angiotensin-converting enzyme (ACE) 2 receptor, in order to enter the target cells. These receptors are abundant in the epithelial cells of many human tissues – the lung, intestine, heart, kidneys, and blood vessels. There is also another form of ACE2, a soluble one which is found in the blood.
ACE2, like ACE, splits angiotensin I to angiotensin II, to attach to and activate the angiotensin II receptor, leading to vasoconstriction, inflammation, and oxidation. Unlike ACE, however, it also breaks down angiotensin II to two other molecules, one of which has anti-inflammatory, antioxidant, and vasodilatory effects.
RAS inhibitors, which include both ACEIs and ARBs, are considered to have a beneficial impact on heart failure, hypertension, and ischemic heart disease.
One group of researchers points out that patients who are treated with ACEIs or ARBs have a higher expression of ACE2. This could lead to an increased risk of infection with the virus.
On the other hand, some researchers have found a higher level of angiotensin II in the blood of COVID-19 pneumonia patients. They think the binding of the virus to these receptors may reduce the activity of the residual enzyme, causing the ACE/ACE2 ratio to become imbalanced. This could increase the level of activity of angiotensin II, causing inflammation and injury to the lung and thus potentially increasing the risk for acute lung injury (ALI), which is so often fatal in this condition. In this case, ACEIs/ARBs could reduce this risk. By their anti-inflammatory effects, they could also prevent the cytokine storm and hyperinflammatory response that drives the acute respiratory distress syndrome (ARDS).
Some scientists also wonder if these drugs could inhibit viral entry into host cells by increasing the levels of soluble ACE2, which would compete with the virus for the receptors and possibly prevent lung injury.
What does existing research say?
Several small studies of varying design have also shown that the use of these drugs improves some outcomes in seriously sick patients with COVID-19. A meta-analysis of 37 studies showed a lower risk of pneumonia and deaths related to pneumonia in patients who were on ACEIs or ARBs.
Another small double-blinded randomized controlled trial showed fewer days on ventilatory support and more days alive outside the intensive care unit with the administration of an ACEI.
A retrospective study from Korea has shown that patients with ARDS had a higher chance of survival if they were on ACEIs or ARBs.
What is the consensus regarding their use?
An array of professional societies have issued their guidelines on the use of these RAS inhibitors in patients at risk of or infected with COVID-19. In essence, all of them say that patients on these drugs should be advised to continue with them unless there is an apparent clinically dictated reason to change them. On the other hand, patients with COVID-19 but without hypertension, diabetes or heart failure, or other clinical condition in which these drugs would otherwise have been prescribed, should not be started on these drugs since there is a lack of reliable supporting evidence as to their benefit.
Future research
The link between the biological mechanisms through which these drugs act and the virus receptor in COVID-10 has aroused scientific curiosity. As a result, several trials are being planned to test the effect of specific drugs in infected patients who are not sick enough to be hospitalized, as well as infected in-patients. More trials will be urgently required to identify if the use of these drugs can bring down the mortality due to ALI or ARDS in COVID-19, irrespective of whether these drugs would otherwise have been prescribed.
Journal reference:
Bavishi, C., et al. (2020). Coronavirus Disease 2019 (COVID-19) Infection and Renin Angiotensin System Blockers. JAMA Cardiology Published online April 3, 2020 doi:10.1001/jamacardio.2020.1282