The COVID-19 pandemic has forced clinicians and academicians to intensive research to find evidence for many conventional therapies. A new round-up editorial published in the journal Cardiovascular Research in April 2020 summarizes the current clinical grounds for and against the use of the commonly used angiotensin axis inhibitors in patients with COVID-19.
A major clinical controversy centers on the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs). Clinicians debate whether their use is detrimental or beneficial in treating COVID-19.
Both ACE inhibitors and ARBs are extensively used at present to treat high blood pressure and reduce cardiovascular risk. Some physicians suggest stopping their use over concerns that it may up-regulate the ACE2 receptor, which acts as an entry point for SARS-CoV-2, the virus responsible for COVID-19. A different group suggests prescribing them to correct the imbalance in the angiotensin-aldosterone system.
The paper explores the links between the renin-angiotensin-aldosterone system (RAAS) and the ACE2 receptor, specifically, based on the observation that hypertension is prevalent in COVID-19 patients.
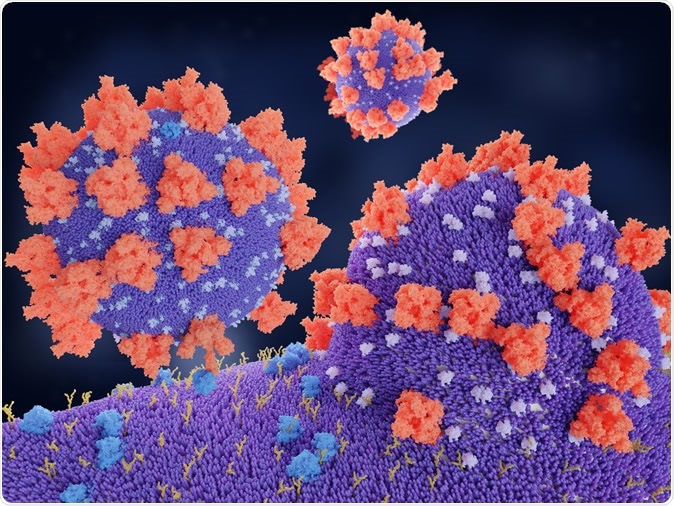
Coronaviruses penetrating in human cell. Binding of the coronavirus spike protein(red) to an ACE2 receptor (blue) leads to the penetration of the virus in the cell. 3d rendering. Image Credit: Juan Gaertner / Shutterstock
The virus
The SARS-CoV-2 virus enters the host cell through the high-affinity binding between its outer S (spike) protein and the catalytic domain of the ACE2 receptor. Pneumocytes (surface cells in the alveoli, the part of the lungs that take part in gas exchange) are particularly likely to get infected because of their high ACE2 content.
ACE converts the molecule angiotensin I (Ang I) to Ang II. This happens chiefly in the lungs. Ang II has to bind to specific receptors to take effect. The binding to AT1 receptors is responsible for the well-known range of effects of Ang II, from increased oxidative stress to vasoconstriction, while AT2 has opposite effects, in principle. SARS-CoV-2 competes with Ang II to bind to ACE2 receptors.
The receptor – ACE2
ACE2, an enzyme that is bound to cell membranes in the lungs, endothelium, heart, and kidneys. Its main effect is a reduction in blood pressure through vasodilation. It also has an anti-inflammatory effect.
It accomplishes these effects by significantly enhancing the splitting of Ang I and Ang II into two shorter peptides called Ang 1-9 and Ang 1-7, respectively. It also binds other substrates that produce vascular effects, such as apelin-13 and bradykinin.
There is also a soluble circulating form of ACE2 that has been split off the cell surface but retains its ability to catalyze angiotensin conversion reactions.
Men tend to have higher ACE2 levels than women. ACE2 lowers blood pressure by catalyzing the hydrolysis of angiotensin II (a vasoconstrictor peptide) into angiotensin (1–7) (a vasodilator).
How is ACE2 related to cardiovascular risk?
In healthy individuals, levels of ACE2 in the blood are low but rise in patients with heart failure, atrial fibrillation, and kidney disease. Various studies have pointed to this conclusion, with higher 10-year major adverse cardiovascular events (MACE), hospitalization due to heart failure, post-operative cardiac events in orthopedic patients, hypertension, impaired left ventricular systolic function, and older age is linked to higher ACE2 levels and activity.
Do ACE inhibitors and ARBs increase the expression of ACE2?
The role of drugs acting on the RAAS and their potential to enhance the risk of serious COVID-19 symptoms by increasing virus entry are some critical questions facing clinicians.
Scientific evidence for the up-regulation of ACE2 arises from animal studies. Rats on an ACE inhibitor demonstrated a drop in circulating Ang II, higher levels of synthesis of ACE2 as suggested by increased ACE2 mRNA, and higher plasma Ang 1-7 levels. The last two effects were also observed with ARB administration. However, there is also evidence to the contrary, with ramipril failing to increase ACE2 levels in a similar experiment.
A group of researchers postulates that ARBs could hinder the entry of the virus into the host cell by reducing the number of binding sites available and the internalization of ACE2, presumably along with the bound virus. However, the effect of ARBs on the breakdown of Ang II is unknown. Moreover, the virus needs only one receptor to infect the cell.
The researchers point out, “There has not been any good evidence of ACE2 up-regulation associated with these drugs in humans.” Moreover, even though ACE1 and ACE2 have similarities over more than 61% of their sequence, ACE inhibitors do not affect ACE2 receptors. It should not be overlooked that animal studies have focused mostly on the tissue levels of ACE2 but human studies on soluble or circulating ACE2. Again, mice and rats are not intermediate hosts of SARS-CoV. These factors preclude a direct comparison or extrapolation of such data to humans since their relationship is not well-established.
Dysregulation of Ang II
Many patients with COVID-19 have been reported to develop hypokalemia (low potassium). This is not due to any apparent loss through the gut and is proportional to the severity of the disease. However, the report on this condition did not mention the prevalence of the use of RAAS inhibitors as a confounding factor.
Some see this as a complication of RAAS dysfunction in COVID-19. They suggest that the loss of potassium through the kidneys may be due to higher Ang II levels due to the binding of the SARS-CoV-2 virus to ACE2 receptors. This could, they think, prevent the action of ACE2 in maintaining the balance between ACE2 and Ang II levels. The ARB losartan was found to improve lung injury in mice by reducing levels of Ang II. When the genes for ACE2 are not expressed in a mouse model, and the knockout mouse, as it is called, is exposed to viral influenza, the affected mice were sicker and less likely to survive. This could indicate the protective role of ACE2 in stabilizing Ang II levels, converting the latter to Ang 1-7.
How viral pneumonia patients react to ACE inhibitors/ARBs
A study on 539 viral pneumonia patients found that using ACE inhibitors increased the risk of death or need for intubation. However, the study did not specify which demographic and clinical features were associated with the use or stoppage of these drugs. It is already known that patients with cardiovascular disease are more likely to use ACE inhibitors, which is already a risk factor for death. Secondly, patients with severe and deteriorating conditions are more likely to stop these drugs. This, again, disproportionately weights this category with adverse odds.
How do COVID-19 patients fare on long-term follow-up?
Long-term outcomes of the disease remain largely unknown. Compared to healthy controls, and those with bacterial pneumonia, lipid metabolism of patients with SARS was found to remain altered even at 12 years follow-up, though this was attributed to the use of the powerful glucocorticoid methylprednisolone as well. Compared with healthy controls, they were found to be more likely to develop cardiovascular and glucose metabolism abnormalities and to require further hospitalization.
What is the conclusion?
Stopping ACE inhibitors and ARBs involves high morbidity and mortality risks, especially since COVID-19 is known to cause heart damage.
Keeping that in mind, several research groups, including the American College of Physicians, Canadian Cardiovascular Society, European Society of Cardiology Council on Hypertension, European Society of Hypertension, Hypertension Canada, International Society of Hypertension and The Renal Association (UK) have opted to support continued ACE inhibitor and ARB use in COVID-19 patients, unless an alternative clinical reason is present that warrants discontinuation.
Journal reference:
Murray, E., Tomaszewski, M., and Guzik, T. J. (2020). Binding of SARS-CoV-2 and angiotensin-converting enzyme 2: clinical implications. Cardiovascular Research, cvaa096, https://doi.org/10.1093/cvr/cvaa096. https://academic.oup.com/cardiovascres/article/doi/10.1093/cvr/cvaa096/5821240