Even as the COVID-19 pandemic continues to wreak disease and death across much of the world, researchers are working overtime to find a cure as well as answers to some practical problems they face during the care of sick patients with multiple underlying risk conditions. Among them, hypertension is a common denominator in many of these cases.
The body is well adapted to deal with constantly and severely changing conditions. One way in which it does so is by maintaining a stable heart rate, blood pressure, and blood flow to its organs. This involves a precise and sensitive regulation of multiple cardiovascular factors.
The renin-angiotensin-aldosterone axis (RAAA) is one of the multiple inputs into this process. It hinges on an enzyme called angiotensin-converting enzyme (ACE), which converts angiotensin into angiotensin II. This is a potent vasoconstrictor, raising blood pressure and increasing oxidative stress via its action on the AT1 receptor.
It is thought that this is antagonized by the vasodilator and anti-inflammatory action of Ang I and Ang II cleavage products, catalyzed by the second enzyme ACE2. This molecule is found all over the body, in a wide variety of tissues, and is the entry point for the SARS-CoV-2 into the human cell.
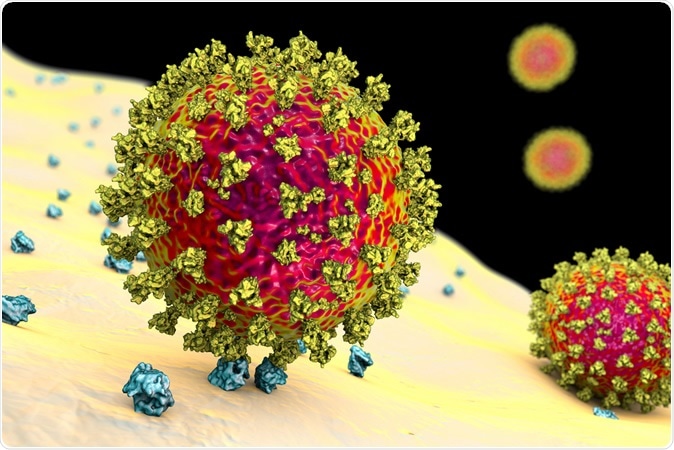
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection, conceptual 3D illustration credit: Kateryna Kon / Shutterstock
The role of cardiovascular and metabolic disease in COVID-19 mortality
Among the over 170,000 fatalities caused by COVID-19, the vast majority have been in people over the age of 50 years, and especially over 70 years. One major factor for this many-fold increase in the risk of fatal complications is the presence of underlying hypertension and vascular obstruction. Thus it becomes a matter of the most significant importance to manage the blood pressure correctly while the patient is affected by COVID-19.
ACE inhibitors and angiotensin receptor blockers (ARBs) have been extensively used in the management of hypertension. However, since the ACE2 receptor is the entry point for the novel coronavirus, much controversy surrounds the use of these drugs in patients with COVID-19. This is because drugs that modulate the RAAA could perhaps increase the rate of expression of ACE2, providing the virus with more entry points and increasing the risk of severe disease – thus goes the hypothesis.
On the other hand, there is no evidence that ACE2 is inhibited by clinical doses of the ACE inhibitors or ARBs. Moreover, these drugs act in different ways to regulate the ACE2 enzyme, depending on the tissue of origin.
The Zhang study conclusions
A study by Zhang et al. published in the same journal reports a retrospective analysis of over 3,000 patients with COVID-19 in Hubei, China. This included over 1,100 patients with high blood pressure. All cases were confirmed, and the individuals already sick with other illnesses were excluded.
The researchers looked at the 28-day mortality as the primary outcome. The researchers found that, like some earlier studies, higher blood pressure led to more severe illness and higher mortality. They compensated for an array of confounding factors, including age, sex, the presence of inflammation, and certain underlying diseases. They found that patients who received ACE inhibitors or ARBs currently or had been on these drugs in the past were less likely to develop a severe illness or to die.
Limitations of this study
The authors point to several limitations of the Zhang study. For one, it is an observational and a retrospective study, which means it cannot assign a causative role to any observed association. Secondly, unknown confounding factors could have affected the outcome as it is not a randomized trial. It is possible that patients who were on ACE inhibitors for a longer duration beforehand had a different degree of expression of ACE2 compared to those who had used them only for a short period.
A possible mechanism for the protective effect of angiotensin axis blockade
Despite these limitations, there are plausible reasons why these drugs might not harm, and might benefit, COVID-19 patients by blockading the RAA. It is known that once the SARS-CoV-2 enters the host cell, it brings down the level of ACE2 expression on the cell. The extent to which ACE2 is suppressed may determine the severity of the resulting lung injury.
For instance, if there is a complete absence of ACE2, following viral entry, the circulating level of Ang II goes up, causing pulmonary injury in a bird flu model. In a mouse model, infection with the virus causes the level of ACE2 in the heart to drop. People with SARS-CoV-2 show the same trend, with higher myocardial inflammation levels. This is similar to and recorded since the earlier SARS epidemic. This has sparked new interest in experiments with losartan in COVID-19, and in the use of recombinant ACE2 to regulate the RAA.
Conclusion: continue ACE inhibitors/ARBs unless otherwise indicated
The study, say the expert commenters, "is a hypothesis-generator and should not be used to guide the choice of therapeutic modality. It also doesn’t offer any help with understanding how drugs modulating the RAAA act to worsen or improve the condition; the retrospective data does offer support to currently ongoing randomized controlled trials of these drugs."
The take-home is simple: “Currently, outside of clear clinical indications to stop these medications that have existed long before the current pandemic, the withdrawal of these medications in the context of those conditions in which they have a proven benefit (e.g., heart failure with reduced left ventricular ejection fraction) may actually inflict more harm than good.”