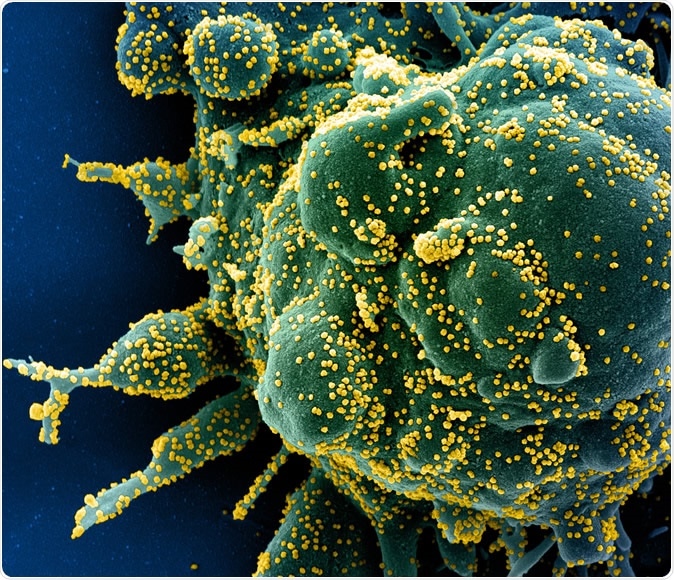
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Plasma concentration of ivermectin
The in vitro study used ivermectin at a concentration that inhibits 50% of proliferating viruses (IC50). This concentration of 2 μM is 35 times higher than the maximum plasma concentration achieved in blood on oral administration of ivermectin at the approved dose of approximately 200 μg/kg. And this refers to the total plasma concentration.
Ivermectin is bound extensively by plasma protein, to the tune of 93%, which means that the maximum concentration of unbound ivermectin in the plasma is several orders of magnitude less.
When oral ivermectin is administered in humans, it reaches the lungs in unbound form, and the final concentration also depends on the presence of specific transport proteins that can keep the drug in the lung tissue, as well as how rapidly it binds to and crosses the fatty cell membrane of the cell.
Unrealistic dosing
The actual concentration in the human lung cannot be measured. In cattle experiments, a single dose was shown to produce lung levels almost three times higher than the total plasma level. Despite this, lung ivermectin concentrations are “unlikely to reach the IC50 after oral administration of the approved dose in humans,” say the researchers.
Ivermectin has a wider therapeutic margin, allowing some increase in the dose if warranted, without unduly pushing up the risk of toxicity. This has led to the evaluation of higher than usual doses of ivermectin in a phase 3 trial to assess the safety. Another phase I trial looked at doses, 10-fold the approved dose.
The results showed the drug was tolerated with the ten-fold dosing regime as well as at 60 mg three times a week.
How was the study done?
The current study was aimed at analyzing the human dose necessary to achieve the experimental IC50 in the lungs. This is crucial to planning a clinical trial.
The researchers used a population model to study the pharmacokinetics of the drug. This included the transit absorption, drug elimination, and weight of the patient. The model was based on healthy participants who took 12 mg ivermectin orally after food.
A hundred simulations of total and bound ivermectin were performed to track the total plasma concentration-time profile. Different doses were used, such as the approved dose of 200 μg/kg, 120 mg in a single weekly dose, and 60 mg three times a week (at 72-hour intervals, in healthy subjects).
These additional simulations were carried out because of the observation that after a subcutaneous dose, ivermectin levels remained stable in cattle lungs for eight days. They then declined slowly over 30 days.
The concentration-time graph for unbound plasma ivermectin was also predicted from the data. Maximum total plasma concentrations were derived.
What did the results show?
The researchers found that the plasma concentrations, whether of total, bound, or unbound ivermectin did not reach the IC50 even with a tenfold rise in the dosage or after repeated dosing. The lung concentration in cattle is 2.7 times higher than in plasma, but even so, lung concentrations fall short of the IC50 of 2 μM.
To reach this level, ivermectin would need to accumulate in the lungs more than 25 times the calculated rate at the approved weekly dose. For the weekly 120 mg dose, it would need to build up over 2.5 times. With the 72-hourly dosing of 60 mg, it would have to rise to 5 times the observed level.
The estimated accumulation ratio in the lung tissue is 2.20, which results in lung concentrations reaching only a tenth of the IC50 at the approved dose given three times a week. Even with daily dosing at approved doses, it rises to only a fourth of the IC50
What are the implications of the study?
The current approach to finding a viable therapy for the SARS-CoV-2 is to repurpose existing drugs. All over the world, ivermectin came into widespread use of off-label in response to the news of the in vitro success against the virus.
At a dose of 150 μg/kg, observation of 52 patients on mechanical ventilation appeared to show clinical benefit with the drug in contrast to over 1,900 patients on conventional treatment. Though these results need to be analyzed to rule out confounding factors and biases, on the surface, they would seem to suggest that very low lung concentrations of ivermectin are able to inhibit the virus.
In other words, even when the ivermectin concentration is not anywhere near the IC50, it appears to have antiviral activity. This could suggest that the lung distribution or accumulation of this drug is far greater in humans than in cattle.
In contrast, the concentrations of ivermectin reported inhibiting the coronavirus in vitro were markedly higher than those achieved in human lung or plasma with the approved doses of ivermectin. As a result, say the researchers, “the likelihood of a successful clinical trial using the approved dose of ivermectin is low.”
This should be a warning to conduct in vitro studies of repurposed drugs at concentrations that are safe and tolerable in humans.
Future recommendations
The researchers advise a dose-response study using a control group, as well as testing the possibility of inhaled ivermectin and combination therapy.
The dose-response study should begin with the addition of potentiating compounds to reduce the threshold of viral inhibition to the tune of 0.1 μM rather than the 5 μM of the original experiment. Close monitoring is required since these dosage levels and protocols have not been widely studied.
Inhaled ivermectin would allow for higher dosage and increased local lung concentrations without additional systemic exposure. However, preclinical studies of its safety and tolerability are required.
The study sums up: “Ivermectin is unlikely to reach the IC50 in lungs after oral administration of the approved dose or doses 10x higher than the approved doses as a single dose. The approved dose of ivermectin alone has a low probability of success in the treatment of COVID-19.”
Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Correction
It has come to our attention that the original title of this article, "Ivermectin alone not useful in treating COVID-19" was inadvertently misleading. The title has been corrected to better reflect the research paper's title, "The Approved Dose of Ivermectin Alone is not the Ideal Dose for the Treatment of COVID-19".

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources