The current study from the Cleveland Clinic Health System investigated the effects of angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) on the outcome of tests for COVID-19, as well as the severity of disease and clinical outcomes. The study did not find any significant association between the use of ACEIs or ARBs and COVID-19 test positivity.
To date, ACEIs and ARBs are prescribed for the management of chronic illnesses like hypertension and heart disease. However, in the light of the recent COVID-19 pandemic, some researchers fear that their use might exacerbate disease symptoms. This is founded on data from animal studies, which shows that ACEIs and ARBs enhance the expression of membrane-bound angiotensin-converting enzyme 2 (ACE2), which is the viral receptor for the human cell.
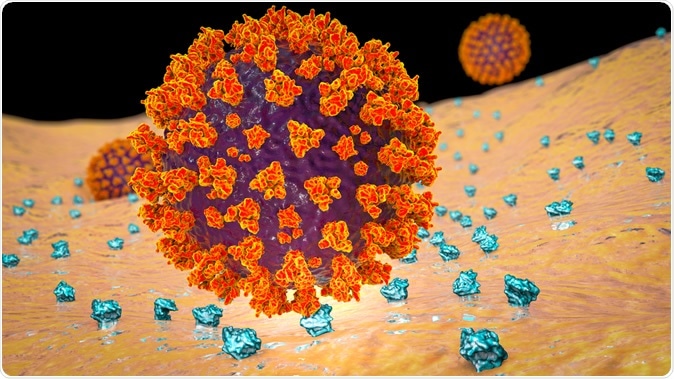
SARS-CoV-2 virus binding to ACE2 receptors on a human cell, the initial stage of COVID-19 infection, illustration credit: Kateryna Kon / Shutterstock
By enabling the entry of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) into cells, in theory, these drugs might increase the risk of severity for COVID-19 patients.
On the other hand, angiotensin II is converted to angiotensin (1-7), which has potential vasodilatory and anti-inflammatory properties through ACE2 binding. In this case, the upregulation of ACE2 is seen as a potential benefit for COVID-19 patients.
Professional societies recommend that those who are already on these medications continue taking them, as their withdrawal could be harmful in certain high-risk patients. Clinical evidence for either approach is insufficient at present.
How was the study done?
The retrospective cohort study was undertaken in the Cleveland Clinic Health System in Ohio, and Florida, including all patients, tested for COVID-19 from March 8, 2020, to April 12, 2020. The study investigated the likelihood of ACEI or ARB users testing positive for SARS-CoV-2 infection, and their clinical disease outcomes, as assessed by hospital admission, ICU admission, and requirement of mechanical ventilation during the patient's first hospitalization.
A total of 18,472 patients who were tested for SARS-CoV-2 were included, with a mean age of 49 years. Out of them, 1,322 were taking ACEIs and 982 were taking ARBs - together, around 12% of the tested population was on either ACEIs or ARBs. Most of the tested population had co-morbidities - hypertension, coronary artery disease, chronic, obstructive pulmonary disease, and heart failure.
Out of the 18,472 tested for SARS-CoV-2, 1,735 patients tested positive. Of these, 116 were taking ACEIs, and 98 were taking ARBs or about 12%.
Do these drugs cause a higher likelihood of disease or more severe illness?
Researchers stated that taking either an ACEI or ARB did not increase one's chances of testing positive for SARS-CoV-2 infection. After adjusting for confounding factors, the test positivity rate among patients on these drugs was 8.6%, and 10%, for those on ACEIs and ARBs, respectively, as compared to 9.5^ and 9.3% in those not on these drugs.
Although initial unadjusted analyses showed worse clinical outcomes for patients taking either ACEIs or ARBs, researchers noted that the medications were often prescribed for underlying chronic disease conditions, which would increase the risk of disease severity.
Further analysis showed a higher likelihood of hospital admission among patients who were on either ACEIs or ARBs. Patients who were taking ACEIs were reported to have a higher likelihood of ICU admission. However, the use of ARBs was not associated with increased ICU admissions. Neither ACEI nor ARB use was associated with an increased requirement of mechanical ventilation during the hospitalization episode included in the study.
What does the study imply?
Researchers warned that the limitations of the study did not permit large-scale generalization of the findings, recommending further research on the effects of the drugs on disease outcomes, with larger datasets.
They did conclude that the findings appeared to support the recommendations of various professional societies, which recommend continued use of the drugs, especially for those with chronic diseases.
"At present, there is no convincing evidence that ACEIs/ARBs have effects on the transmembrane ACE2 receptor in humans that would predispose to COVID-19 infection," the study says.
Journal reference:
Mehta N, Kalra A, Nowacki AS, et al. Association of Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers With Testing Positive for Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. Published online May 05, 2020. doi.org/10.1001%2Fjamacardio.2020.1855