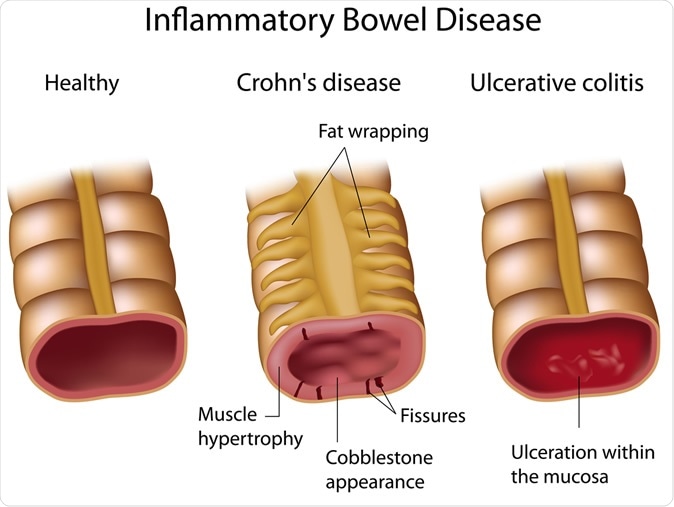
Crohns and Ulcerative colitis. Image Credit: Alila Medical Media / Shutterstock
This was part of the National Health Interview Survey 2015 that looked at the prevalence of inflammatory bowel disease (IBD) among US adults and the frequency of consumption of certain foods.
The researchers wrote that several foods had been associated with worsening of symptoms of IBD, and there are environmental factors that are known to affect the outcome and course of IBD. They explained that patients are also recommended to follow certain guidelines regarding their diets to help them keep their disease symptoms under control. The team wrote, "However, the current food consumption pattern of U.S. adults with IBD that are nationally representative is unclear."
IBD encompasses two inflammatory conditions of the gut – ulcerative colitis and Crohn's disease. According to the Centers for Disease Control and Prevention (CDC), these chronic inflammatory conditions affect nearly three million American adults. There are symptoms including diarrhea, bleeding with stool, abdominal cramps, malnutrition, weight loss, and general weakness. These symptoms can be "increasingly debilitating, potentially reducing the quality of life and the ability to thrive physically and socially," write the researchers.
The Crohn's & Colitis Foundation guidelines suggest that fibers, whole grains, fruits and vegetables, calcium, and protein in diet along with fluids are necessary to manage the symptoms of IBD. The authors of the study write that foods such as those with high "total fat, polyunsaturated fatty acids, omega-6 fatty acids, saturated fats, and meats" are known to raise the risk of worsening of symptoms of IBD. Dietary fiber and fruits can reduce the symptoms of Crohn's disease but do not affect Ulcerative colitis. They explain that the western lifestyle and dietary patterns are often associated with an increased incidence of IBD. They wrote, "a definitive role of various food intake in disease etiology or symptom management still needs much elucidation," and thus they conducted this study.
What was done?
This was part of the National Health Interview Survey 2015 (NHIS) and assessed the food frequency and pattern of diets focusing on 26 types of foods. The NHIS has a supplement assessment " quinquennial Cancer Control Module (CCM)," they wrote, and this was essentially a household survey conducted annually since 1960.
Participants were given questionnaires with six sections, "Household, Family, Person, Sample Child, Injury Episode, and Sample Adult." For the participants, age, ethnicity, educational level, family income, locality of residence, and socioeconomic variables were taken into account. For each of them, body mass index (BMI, kg/m2), smoking status, and alcohol use level were also recorded.
Food items assessed included:
- cereal (hot or cold)
- popcorn, brown rice (and other whole grains)
- whole-grain bread
- fries (or any other fried potatoes)
- salad (including green leaf or lettuce of any kind)
- 100% pure fruit juice
- vegetables
- non-fried potato
- pizza
- fruits
- tomato sauce
- salsa (made with tomatoes)
- beans
- milk (from a cow)
- cheese (excluding cheese from pizza)
- ice cream (or frozen desserts)
- processed meat
- red meat
- cookies (including pies, cakes, brownies)
- donuts (including pastries and muffins)
- candy (including chocolate)
- sports and energy drinks
- regular soda (or pop)
- coffee or tea (sweetened with sugar or honey)
- fruit drinks (sweetened with sugar)
Food consumption recall for the past 30 days was self-reported and recorded. Outcome variables of the study included health assessments, including questions such as, "Have you ever been told by a doctor or other health professional that you had Crohn's disease or ulcerative colitis?"
What was found?
Results showed that fries were consumed by a large number of patients with IBD, as were cookies, cheese, and soda or energy drinks compared to those who did not have IBD. They also drank less of 100 percent fruit juice, the study noted. They also noted that those who took more fries, sports drinks, and soda were more likely to have worse symptoms of IBD, the researchers noted. The risk of symptoms was not worsened much by the consumption of popcorn and milk. The team wrote, "Foods typically labeled as junk food was positively associated with IBD."
Conclusions and implications
First author of the study, Dr. Moon Han, working as a Ph.D. student in Dr. Didier Merlin's lab in the Institute for Biomedical Sciences and now works as a Health Scientist ORISE Fellow at the CDC said, "While foods typically labeled as junk food was positively associated with inflammatory bowel disease, we found the eating patterns of people with and without this disease to be very similar. However, it's unclear whether the survey results reflect a potential change in the food intake of people with inflammatory bowel disease long before the survey was conducted."
The authors wrote in conclusion, "Understanding the role of food intake in IBD risk/prevalence would benefit from identifying other environmental factors (i.e., food desert), food processing (i.e., frying), and potential bioactive food components that can induce intestinal inflammation that can increase the individual's susceptibility to IBD."
Journal reference:
- Examination of food consumption in United States adults and the prevalence of inflammatory bowel disease using National Health Interview Survey 2015 Han MK, Anderson R, Viennois E, Merlin D (2020) Examination of food consumption in United States adults and the prevalence of inflammatory bowel disease using National Health Interview Survey 2015. PLOS ONE 15(4): e0232157. https://doi.org/10.1371/journal.pone.0232157