When severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infects the host, the immune system begins to respond. At this stage, drugs that can reinforce or boost the innate or adaptive response are essential to keep the infection mild and avoid its spread to other parts of the body. Once the infection has taken hold, the cytokine storm that sets in with some individuals can cause multi-organ dysfunction and severe respiratory distress. At this point, drugs that can modulate the immune system and prevent organ damage due to hyperactive inflammatory processes are important.
As a result of this knowledge, several drugs that are in use to treat inflammatory and autoimmune disorders have been studied to see if they can be repurposed to treat severely ill COVID-19 patients.
The Role Of ACE2
The angiotensin-converting enzyme 2 (ACE2) is a transmembrane protein that serves as one of the receptors for the virus that causes COVID-19. This protein is abundantly expressed on some lung cells, including the type II alveolar cells. This may be why these are so vulnerable to injury in this illness.
ACE2 also plays an immunomodulatory role, which is why the reduced expression following the entry of the virus can result in acute respiratory distress syndrome (ARDS).
The Inflammatory Response
Like other betacoronavirus pneumonias, COVID-19 in the lungs also induces an inflammatory response as a result of T cell activation, both CD4 and CD8 cells, along with monocytes and natural killer (NK) cells.
These cells secrete a multitude of cytokines and chemicals, including IL-2, IL-7, TNF-α, and G-CSF, the levels of which are higher in sicker patients. The Janus Kinase (JAK) inhibitor (JAKi) pathway is therefore useful in dialing down the level of injury by restraining cytokine signaling via a reduction in JAK-dependent molecules like IL-6.
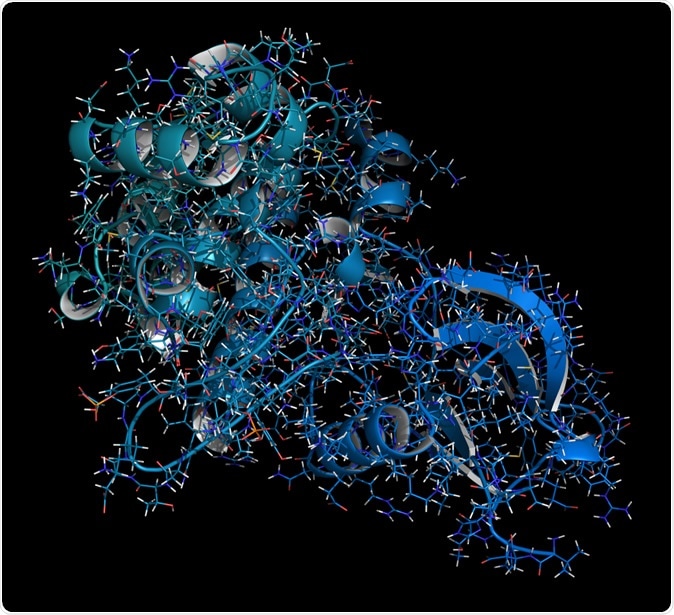
Janus kinase 1 protein. Part of JAK-STAT signaling pathway and drug target. Image Credit: StudioMolekuul / Shutterstock
High levels of IFN-γ and other cytokines in the tissue rather than the blood downregulate ACE2 expression and drive the progression of pneumonia. Other molecules like IL-1β, IL-6, and IL-12 seem to drive the cytokine storm through the activation of NK and Th1 cells, to release the chemokines which attract more inflammatory and immune cells, intensifying the lung inflammation.
Baricitinib – a JAK inhibitor
One possible candidate for JAKi therapy is Baricitinib, a synthetic disease-modifying anti-rheumatic drug used in rheumatoid arthritis (RA). This first-generation JAKi blocks the activity of both JAK1 and JAK2. This may result in the inhibition of many other kinases in the numb-associated kinase (NAK) family, which are involved in endocytosis, the process by which the virus enters the host cell.
It is, therefore, possible that baricitinib could not only calm or prevent the cytokine storm but also block the early stages of viral entry and spread into the host cells. Simultaneously, IL-4 and IFN-γ, which are both JAK-dependent cytokines have been found in vitro to block the expression of the ACE2 receptor, reducing the likelihood of infection and replication.
Clinical trial findings
Several trials have looked at the role of baricitinib or other JAKi. The first to report the findings is a trial at the Hospital of Prato in Italy, which conducted an open-label trial.
The participants here were 24 COVID-19 cases in hospital with mild to moderate pneumonia. All patients were given ritonavir, lopinavir, and hydroxychloroquine as the standard of care. Twelve patients were also given baricitinib for 14 days.
The researchers looked at the percentage of patients on baricitinib who needed intensive care. At the same time, other secondary outcomes included the progression of the disease in clinical terms and any adverse events due to the treatment.
The study showed that patients given baricitinib had significantly larger reductions in fever, breathlessness, and cough, as well as more marked improvements in pulmonary function tests. C-reactive protein levels, which indicate systemic inflammation, were also lower.
None of these 12 patients needed intensive care compared to a third of the controls. At two weeks, 58%, that is, seven of the 12 patients in this group were discharged as recovered, but only 1 of the 12 patients in the other group.
This early evidence of clinical benefit with baricitinib may be explained as due to its blocking viral entry, or its modulation of the excessive inflammation seen in critically ill patients. If the second mechanism operates, circulating CRP levels, at least, must be measured before and after treatment begins, because this compound is linked to IL-6 levels.
Potential Adverse Effects
While it is urgent to find effective therapeutics against this virus, it is also important to ensure that repurposed drugs used extensively to treat such patients are safe. Baricitinib does cause a reduction in NK cell count, which indicates that it can be used for only a short period in COVID-19.
The issues with JAKi must also be considered along with the apparent success of the treatment. For one, these drugs may reactivate varicella-zoster infection in patients with RA. This may signal the inhibition of cytokines like type I IFN, which have antiviral activity.
On the other hand, SARS-CoV-2 can use its own escape route to prevent the IFN pathway from regulating it at an early step. It has genes that encode powerful anti-type I IFN or degrade the transcriptional mRNA for this purpose.
However, this virus does not induce gene expression for IFN or related genes in infected lung tissue, as shown by one study. Secondly, the type I IFN response is prominent in mild to moderate cases, but in severely ill patients, it is suppressed.
Since JAKi inhibits multiple cytokine signaling pathways, the greatest benefit with the use of this drug would be seen in patients who have the highest levels of IL-6 and other inflammatory markers in serum. A comparison of the number of RA patients who are maintained on baricitinib and acquire SARS-CoV-2 and those who are on other DMARDs and acquire the infection should also be helpful in evaluating the possibility of pre-exposure and early post-exposure protection due to the suggested antiviral effect of the drug.
A second potential safety concern is the risk of thromboembolism linked to JAKi use. Patients with critical COVID-19 often have clotting defects, with a poorer outcome. The reasons underlying this effect are still being studied. It could be due to any combination of direct viral endothelial toxicity, the cytokine storm, or antiphospholipid antibodies.
The role of JAKi and other small molecule drugs in stalling the cytokine storm will require more study to validate the current results and determine the right protocol.