At the end of 2019, patients with COVID-19 were diagnosed in Wuhan, China, infected by a SARS-CoV-2. The WHO first declared this outbreak a public health emergency of international concern and subsequently a worldwide pandemic.
So far, COVID-19 has affected nearly four million individuals worldwide and caused more than 270,000 deaths. However, little is known about the protective immune responses induced by SARS-CoV-2. My laboratory has been engaged in immunology research.
In order to understand the immune responses of COVID-19 patients, especially adaptive immunity, we have designed and conducted this study together with our collaborators.
.jpg)
Image Credit: Andrii Vodolazhskyi/Shutterstock.com
Why is it important to understand which cells participate in immune-mediated protection from COVID-19?
Only by understanding which cells are involved in immune-mediated protection, we can design and develop effective COVID-19 vaccines.
Currently, little is known about the immune responses of the body from the SARS-CoV-2 virus. Why is this?
Since SARS-CoV-2 is a brand-new virus, it will take a while for researchers to study and get a comprehensive understanding of it.
Can you describe how you carried out your research into the immune responses of COVID-19?
Firstly, we collected blood samples from 14 mild COVID-19 cases who had recently recovered from the infection. Secondly, we expressed and purified virus-encoded proteins, such as nucleocapsid protein and the receptor-binding domain (RBD) of Spike protein.
Then we measured virus-specific antibody responses via ELISA assay, neutralizing antibody titers via a pseudovirus-based assay, virus-specific T cell responses via ELISpot assay. By these analyses, we found that most discharged patients mount virus-specific antibody and T cell responses.
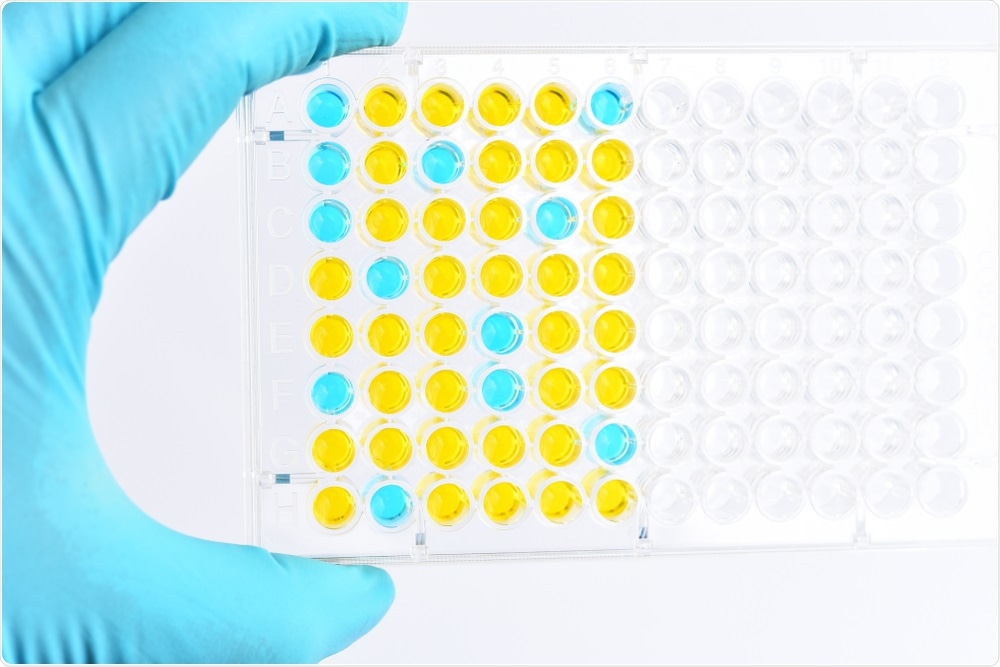
Image Credit: Jarun Ontakrai/Shutterstock.com
What were your findings?
What we found was that most patients who have recovered from COVID-19 produced virus-specific antibodies and T cells. The antibodies were maintained for at least two weeks after discharge. In all 14 patients tested, 13 displayed serum neutralizing activities in a pseudotype entry assay.
Notably, there was a strong correlation between neutralization antibody titers and the numbers of virus-specific T cells.
What role do immunoglobulin antibodies play in immune response?
An antigen is a substance that can invoke an immune response and an antibody to it is a product of the immune system’s response.
Antibodies can directly neutralize the antigen and/or bind to antigens so that scavenger cells would clear them out of the body.
How do patients that have recently recovered from COVID-19 produce virus-specific antibodies and T-cells?
Our immune system is very complex. Just mentioned previously, an antigen is a substance that can invoke an immune response. After the SARS-CoV-2 virus enters our body, it can produce several antigens, some for humoral immunity, and some for cellular immunity.
Once our immune system detects antigens, antigen-presenting cells can take up these antigens, process them, and present epitopes in conjunction with class II or I MHC molecules, which results in the production of virus-specific antibodies and virus-specific CD8+ T cells, respectively.
Why are the immune responses between these patients so varied?
It is not clear why different patients show different levels of immunity.
We speculate that this could be caused by the initial amounts of viruses they encountered, their physical states, or even microbiota.
Could these patients that have developed virus-specific antibodies, be protected from re-exposure to the virus?
If the neutralizing antibody titers in the patients are maintained at a high level, the patients should be protected from re-infection.
Do you believe that your research will help in the development of a vaccine for COVID-19?
Of course, our findings can contribute to the development of COVID-19 vaccines.
An effective COVID-19 vaccine should induce virus-specific antibody and T cell responses.
What are the next steps in your research?
A lot of questions on SARS-CoV-2 remain unknown. For example, we do not know how long the immunity against SARS-CoV-2 can persist.
To address this question, a follow-up study should be carried out. Another one is how the discharged patients who do not produce neutralizing antibodies clear SARS-CoV-2.
If informed consent can be obtained from those patients, the mechanism of action should be investigated. In addition, future studies should distinguish which types of T cells are activated by SARS-CoV-2 infection.
Image Credit: Orpheus FX/Shutterstock.com
Where can readers find more information?
URL: https://www.cell.com/immunity/fulltext/S1074-7613(20)30181-3
DOI: http://dx.doi.org/10.1016/j.immuni.2020.04.023
About Professor Chen Dong
Dr. Dong is Professor and Director of the Institute for Immunology and also Dean of the School of Medicine at Tsinghua University, Beijing, China.
Dr. Dong served as a Professor of Immunology and the Director of the Center for inflammation and Cancer at the University of Texas MD Anderson Cancer Center. Dr. Dong’s research is to understand the molecular mechanisms whereby immune and inflammatory responses are normally regulated and to apply this knowledge to the understanding and treatment of autoimmunity and allergy disorders as well as cancer.
The work from Dr. Dong’s group has led to the discoveries of T cell subsets in the immune system and elucidation of their biological and pathological functions. Dr. Dong has over 200 publications and was rated highly cited researcher for six years from 2014 to 2019.
The honors he has received include the 2009 American Association of Immunologists-BD Bioscience Investigator Award and 2019 International Cytokine and Interferon Society Biolegend-William E. Paul Award.
He is a fellow of the American Association for the advancement of science and a member of the Chinese Academy of Sciences. He is currently an Editor for Immunity, Editor-in-chief for Frontiers in Immunology- T Cell Biology and Associate Editor for China Sciences- Life Sciences.