The purported "game-changer" anti-malarial drug Hydroxychloroquine, which was claimed to be effective in preventing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and also helping better outcomes in COVID-19 patients, seems to have failed in clinical trials.
Researchers writing in the latest issue of The Lancet said that neither Hydroxychloroquine or chloroquine benefitted patients of COVID-19 and even raised the risk of death due to arrhythmias or problems in heart rhythms. The study titled, "Hydroxychloroquine or Chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis," was published in the 22nd May 2020 issue of the journal. The study was funded by the William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women's Hospital.
What was the study about?
The COVID-19 pandemic began in late December 2019 in Wuhan, China, and since then has affected almost all countries around the world. At present, there are no drugs to treat this illness, and no vaccines have been developed to prevent infection. Certain initial small studies had shown the benefits of anti-malarial drugs Hydroxychloroquine and chloroquine in the management of COVID-19 cases with benefits in terms of lowered hospital stay and risk of death. French physician Didier Raoult first began using the drug in Marseille and published a small study in March 2020 regarding its success. However, that study was too small to be of significance, and there was no control group of patients to compare the outcome of the drugs. The World Health Organization (WHO is also conducting a global study called the Solidarity trial to assess the effectiveness of this drug and its combination with a macrolide in COVID-19.
Some studies however, have contradicted the initial hopeful findings. This new study by researchers Professor Mandeep Mehra, Dr. Sapan Desai, Professor Frank Ruschitzka, and Dr. Amit Patel attempted to clear the evidence.
The team wrote that Hydroxychloroquine or Chloroquine had been used in combination with a second-generation macrolide such as Azithromycin in the management of COVID-19. There has been no conclusive evidence regarding the benefits of this combination. They added that both drugs are safe, and the former is considered to be a safe drug when used according to recommendations in malaria and autoimmune diseases. The safety and efficacy of these regimens are not clearly known in COVID-19.
What was done?
This was an international study and a large one to prove without doubt the safety and efficacy of this drug alone or in combination with macrolides in COVID-19. The registry data covered 671 hospitals from six continents, where patients admitted between 20th December 2019 and 14th April 2020 were included in the study. These patients had a positive result for SARS CoV-2 and thus were confirmed patients with COVID-19.
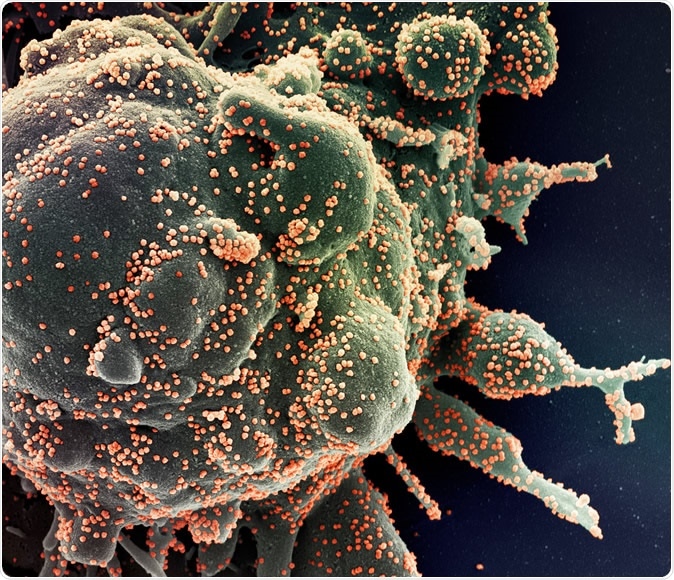
Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (orange), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
All participants of this study received one of the treatments within 48 hours of diagnosis. They were classed into four treatment groups and one control group according to the management they received. These were;
- Chloroquine alone
- Chloroquine with a macrolide
- Hydroxychloroquine alone
- Hydroxychloroquine with a macrolide
- Patients who did not receive any treatment
Some patients were excluded from the study. These patients had one of the following factors;
- Those receiving one of the drugs of interest (Hydroxychloroquine or Chloroquine with or without a macrolide) beyond 48 hours of diagnosis with the infection
- Those who received one of the drugs after mechanical ventilation was started
- Patients who were started on another anti-viral drug Remdesivir
Outcomes measured from the study were mortality after being hospitalized, presence or occurrence of heart rhythm abnormalities such as "de-novo ventricular arrhythmias (non-sustained or sustained ventricular tachycardia or ventricular fibrillation)." Several factors were taken into account before arriving at the conclusions regarding the safety and efficacy of these above drugs. These were age, gender, body mass index, race and ethnicity of the patient, presence of underlying cardiovascular diseases, diabetes, lung disease, immunosuppression, smoking status, etc. The baseline severity of the disease was also taken into account.
What was found?
A total of 96,032 patients were included in the study. Their average age was 53.8 years, and there were 46.3 percent females among the study population. They were classified as follows;
- 1,868 received Chloroquine
- 3,783 received chloroquine with a macrolide
- 3,016 received Hydroxychloroquine
- 6,221 received Hydroxychloroquine with a macrolide
- 81,144 patients were in the control group
Over the course of the study, 11.1 percent or 10,698 patients died during their hospital stay. The risk of death was 9.3 percent among the control group and 18 percent among those on Hydroxychloroquine, 23.8 percent among those on Hydroxychloroquine, and a macrolide, 16.4 percent with chloroquine and 22.2 percent among those on chloroquine and a macrolide. Each of the regimens wrote the researchers were associated with an "increased risk of in-hospital mortality."
The risk of de-novo ventricular arrhythmias during the hospital stay was 0.3 percent among the control group and 6.1 percent, 8.1 percent, 4.3 percent, and 6.5 percent among those taking Hydroxychloroquine, Hydroxychloroquine and a macrolide, Chloroquine, and Chloroquine and a macrolide respectively.
Conclusions and implications
The authors wrote that this study does not show any benefits offered by Hydroxychloroquine or Chloroquine, when used alone or with a macrolide on the "in-hospital outcomes" for patients with COVID-19. They warned, "Each of these drug regimens was associated with decreased in-hospital survival and an increased frequency of ventricular arrhythmias when used for the treatment of COVID-19." They wrote, "These findings suggest that these drug regimens should not be used outside of clinical trials, and urgent confirmation from randomized clinical trials is needed."
Dr. Mandeep Mehra, executive director of the Center for Advanced Heart Disease at Brigham and Women's Hospital in Boston, said, "Not only is there no benefit, but we saw a very consistent signal of harm." He said, "This is the first large scale study to find statistically robust evidence that treatment with chloroquine or hydroxychloroquine does not benefit patients with Covid-19." He added, "Instead, our findings suggest it may be associated with an increased risk of serious heart problems and increased risk of death." He said in warning, "Randomised clinical trials are essential to confirm any harms or benefits associated with these agents. In the meantime, we suggest these drugs should not be used as treatments for Covid-19 outside of clinical trials." The FDA has also issued a warning regarding the use of Hydroxychloroquine outside of clinical trials or hospitals, saying it carries a risk of heart rhythm problems.