Researchers at the São Leopoldo Mandic School of Medicine in Brazil have presented a review of the current data available on the neurological effects of coronavirus disease 2019 (COVID-9).
Paulo Mei and Laura Loeb hope their review will help researchers understand what is known so far about the link between infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the incidence of neurological conditions.
The authors say they would like to emphasize that “due to the rush to gather information that current times require, the majority of articles found and cited are yet to be peer-reviewed and, therefore, modified and corrected.”
The current review is also currently only available as a pre-print but can be accessed in the server medRxiv* while it undergoes peer review.
Neurological involvement is increasingly being reported
SARS-CoV-2 is the latest addition to a list of six other coronaviruses in the Orthocoronavirinae sub-family that can cause harm to people. Two coronavirus of the alpha genera, HCoV-NL63, and HCoV-229E, and four coronaviruses from the beta genera, HCoV-OC43, HCoV-HKU1, SARS-CoV (or SARSCoV-1) and MERS-CoV, complete the list.
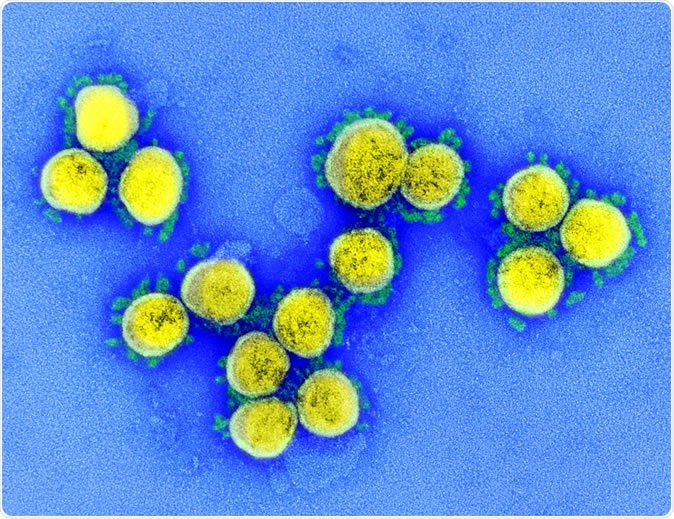
SARS-CoV-2 - Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
An increasing number of reports are describing symptoms beyond the most common ones, such as dry cough, fever, and breathing difficulties. In particular, the evidence points towards a systemic infection that affects various organs and systems throughout the body, including the nervous system.
Mei and Loeb point out that this is not surprising, since other members of the Orthocoronavirinae sub-family, particularly SARS-CoV and MERS-CoV (Middle East respiratory syndrome coronavirus), have previously been reported to have neurological repercussions.
Despite this knowledge, “little is known about potential symptoms and syndromes secondary to the compromise of the central and peripheral nervous systems,” says the team.
A growing number of reports have been describing pathologies of the central nervous system (CNS) and peripheral nervous system (PNS) associated with SARS-CoV-2 infection, as well as other neurovascular conditions. The authors say this highlights the need for more information to help healthcare professionals understand more about what is known so far about these associations.
Now, Mei and Loeb have presented a review of the literature available so far on the neurological manifestations associated with the new coronavirus.
After searching medical databases such as PubMed, PubMed Central, LILACS, and Google scholar, the team identified 41 papers reporting on neurological conditions and COVID-19 (published between late February and mid-May 2020).
What did the study find?
Overall, the articles covered 630 individuals with confirmed COVID-19 and nervous system compromise.
Of those cases, 23 (3.6%) involved the CNS (encephalitis, encephalopathy, and myelitis); 564 (89.6%) involved the PNS (anosmia, Guillain Barré Syndrome, cranial nerve palsy and Miller Fisher Syndrome and muscle lesion) and 43 (6.8%) were neurovascular (stroke).
Five-hundred-and-forty-nine (87%) people experienced anosmia or hyposmia (lost or reduced sense of smell), suggesting that most neurological repercussions are not life-threatening and do not require hospital admission.
However, one to two patients in every ten did experience potentially life-threatening complications, with most of these cases occurring in regions where incidence and mortality were high, including the United States, China, and Western Europe.
The authors say that, currently, it is not clear whether CNS and PNS involvement occurs as a result of direct neuronal invasion and attack by the virus or as a secondary consequence of another event such as a hyperinflammatory response.
Stroke is a major concern
Mei and Loeb say that of all the neurological conditions described, stroke is a primary concern.
“There is at this point a trend in the rise of neurovascular cases, especially stroke from large arteries and to a great extent in young patients,” writes the team. “Although the pathophysiology is still not fully explained, it is known that patients with COVID-19 are prone to hypercoagulability or dyscrasia states.”
Of the 43 cases of stroke, 38 (88%) were ischemic, and the five (22%) remaining cases were hemorrhagic.
“Special attention to immediate care and, to thrombolysis or thrombectomy should be sought in cases of ischemic stroke, especially the ones from large cerebral arteries, prone to graver outcomes and death,” warn the authors.
A broader picture of neurological involvement will emerge over time
In summary, the authors say the data so far suggests that in most (80 to 90%) cases, neurological consequences of SARS-CoV-2 infection are not severe or life-threatening. However, the remaining 10 to 20% can be fatal and may require hospitalization.
“With time, we expect to have a much broader learning of explanations for the causality of neurological symptoms by the new coronavirus,” says the team, due to “more publications and also due to better strength and quality of further published papers, with more detailed and precise descriptions, which tend to be peer-reviewed and vetted.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources