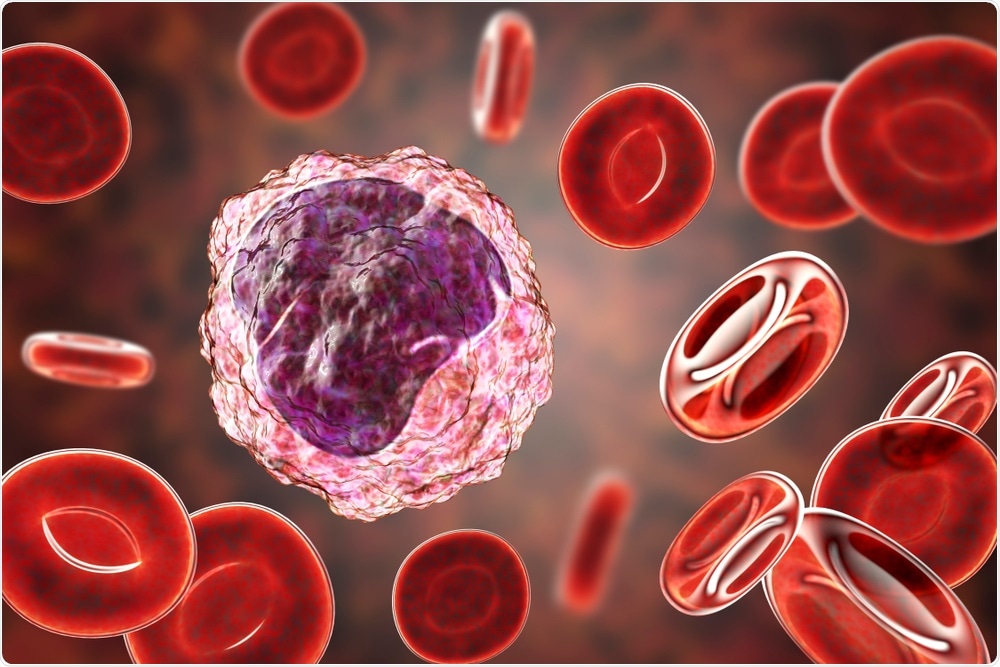
Monocyte surrounded by red blood cells, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
Many studies show that monocytes are probably partly, at least, responsible for the overactive immune response with suppressed T cell activation that is behind the severe lung damage and multi-organ dysfunction often seen with severe or critical COVID-19. This clinical picture resembles that of VAHS, or viral-associated hemophagocytic syndrome, which is serious though an uncommon complication of some viral infections.
VAHS is mediated through the excessive release of inflammatory cell-signaling molecules called cytokines, and the overactivation of macrophages. The excessively high levels of immune activation cause organ damage and sometimes death. The current research aimed at assessing the levels of two blood markers that rise with monocyte activation, namely, sCD14 and sCD163, in COVID-19 patients.
Both CD14 and CD163 are molecules found on monocytes and macrophages, which are, like neutrophils and eosinophils, derived from the bone marrow. The presence of these in soluble form in blood plasma indicates that these cells are activated, and at high levels, they confer a poor prognosis in HIV patients.
The researchers aimed to investigate the correspondence between plasma levels of these soluble markers and the severity of COVID-19, as well as with other inflammatory markers.
The Findings of the Study
The study included 59 COVID-19 patients with confirmed RT-PCR positive infection, 22 of whom were in the intensive care unit (ICU), and 37 who were not, as well as 20 controls of the same age. The serum residuals from routine blood analysis were used for this study. Demographic, treatment, and clinical data were collected from all patients.
The serum samples were analyzed by ELISA for levels of sCD14 and sCD163, along with other laboratory parameters. The researchers found significantly higher levels of both markers among COVID-19 patients, in or outside the ICU setting than in the control group. In the former two groups, the median levels of sCD14 were 2444 ng/mL and 2613 ng/mL, respectively, compared to 1788 ng/mL in the latter. For sCD163, the median levels were 912, 910, and 496 ng/mL, respectively, in the three groups.
They also found that sCD14 and sCD163 levels were correlated significantly with certain clinical measurements in COVID-19 patients in the non-ICU group. These may reflect the use of the IL-6 marker tocilizumab or corticosteroids in the ICU-admitted group. sCD14 levels were positively correlated with ferritin, LDH, C-reactive protein, procalcitonin levels, and negatively with the absolute lymphocyte count, all within the non-ICU group, perhaps because of neither corticosteroids nor Tocilizumab. This marker is also linked to IL-6 levels, which may trigger hyperactive immune responses.
The concentration of sCD163 but not of sCD14was higher with increased time since hospitalization. This could serve as a potential means of predicting disease progression.
This is the first study to show that the concentrations of sCD14 and sCD163 are increased in the blood of infected patients who are hospitalized, though no significant difference was demonstrated in those who required ICU admission.
Implications of the Study
Macrophages and monocytes are important contributors to immune responses. Macrophage-mediated inhibition of the immune response is essential in some viral infections. Higher levels of these markers and the corresponding rise in IL-6 and other inflammatory chemicals underline the strong link between monocyte activation and immune-mediated disease.
IL-6 suppression, by blockading multiple inflammatory pathways, has a good effect on COVID-19 expression. These could, therefore, serve as good therapeutic targets, for instance, by drugs like anti-GM-CSF inhibitors.
The researchers say, “Our results support the hypothesis of a preponderant role for monocytes in SARS-Cov-2 immunopathology, associated with an overexuberant immune response.”
The low sample size, and the use of Tocilizumab and steroids on some students, limit the generalization of the sample. However, the levels of inflammatory biomarkers do suggest that monocytes and macrophages are unduly activated in COVID-19. Larger and broader studies must validate these findings before being taken to shape current clinical recommendations.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources