The novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19 disease first appeared in Wuhan, China, but has spread throughout the world. Its ability to spread rapidly and cause extensive disease, as well as the high rates of spread, make it more deadly even than the earlier SARS-CoV, despite the increased mortality rate associated with the latter.
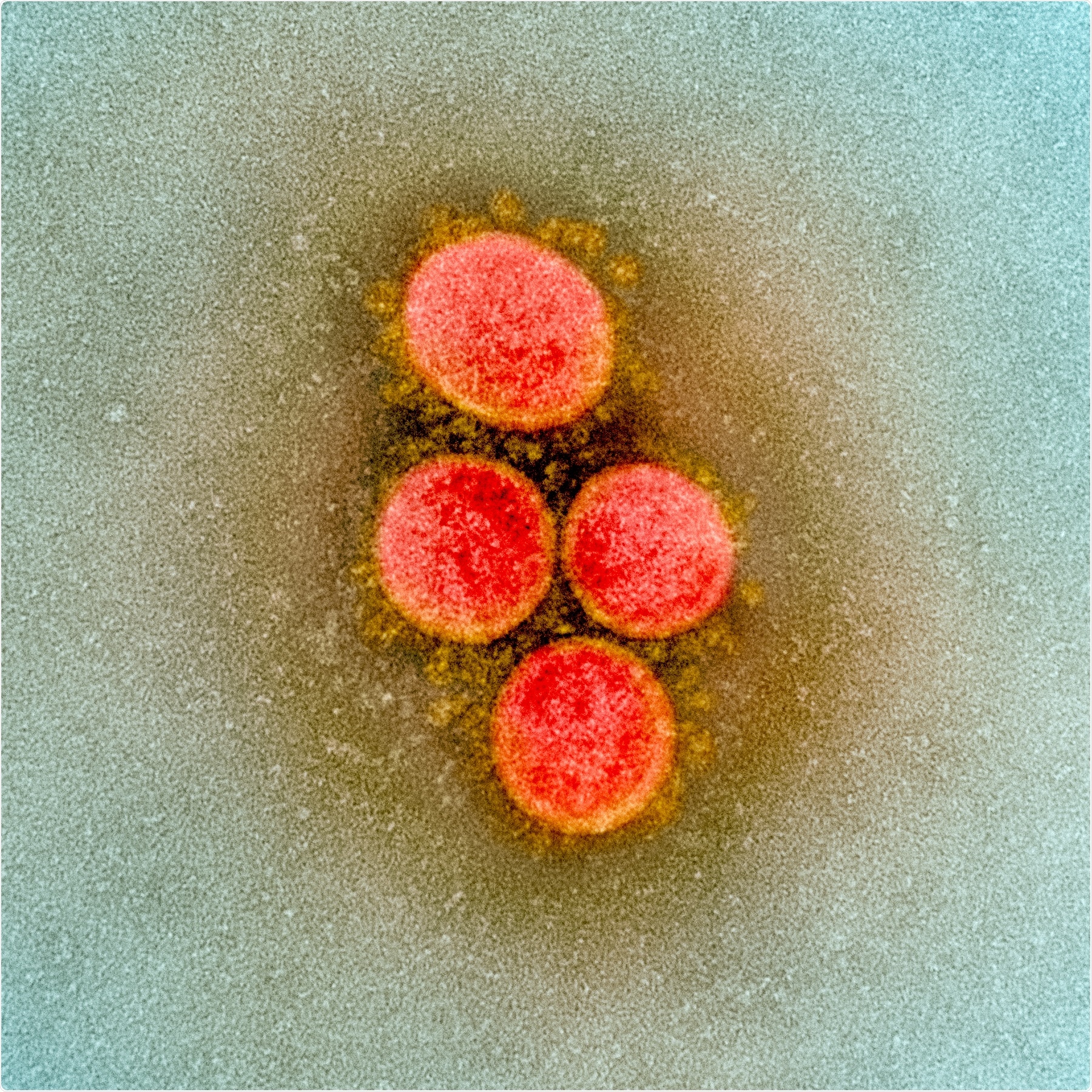
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Predictions about the ultimate cost of the pandemic vary, with some estimating a loss of life in the millions over the next few years. In the absence of known therapeutics or vaccines, scientists are working frenetically to develop effective strategies.
The Spectrum of COVID-19 Disease
In humans, COVID-19 produces a spectrum of disease ranging from asymptomatic to fatal pneumonic illness. The worst outcomes are in people with weakened immunity and other illnesses such as type 2 diabetes.
Non-human primates (NHP) are useful to model the underlying disease process so as to develop effective methods of prevention and treatment. Such models were used to some extent, even with the earlier outbreaks of SARS and MERS. The current study aimed to develop a non-human model to recapture the diversity of human responses to the viral infection and to understand the early events that take place in infected cells in the lungs.
The Acute-Phase Study
The study included three species of NHP, namely, the Indian rhesus macaques, African-origin baboons, and New-World origin common marmosets. The researchers examined the early immune response in the lung cells using high-resolution imaging because of its relationship to disease outcome.
The first step involved a 3-day study of acute infection in four macaques who were exposed via ocular, intratracheal, and intranasal routes, developing signs of infection such as a doubling of the C reactive protein (CRP), reduced serum protein and hemoglobin, and increasing serum CO2 levels. These indicate systemic inflammation, anemia due to viral infection and pulmonary impairment.
Alongside this, there was a fall in the number and relative proportion of neutrophils, probably because these immune cells were recruited to the lung tissue by the infection-associated cellular signals. However, monocytes flooded into the systemic circulation, suggesting that their production in the bone marrow was ramped up by the viral infection. Monocytes are essential for the immune response: their recognition of pathogen-associated molecular patterns (PAMPs) triggers a cascade of cell signals to initiate the interferon-mediated antiviral response.
Macaques, therefore, developed clinical disease with acute infection but no significant weight loss or fever. Bronchoalveolar lavage (BAL), nasal swabs, and nasopharyngeal swabs, as well as oropharyngeal swabs, taken at 1-3 days from infection, showed the presence of viral RNA, whereas it was not detected in similar pre-infection samples. Rectal swabs were positive in only a small sample and only later in the disease course.
Radiographic studies at each day following infection showed progressive abnormalities suggesting multilobar pneumonia on the chest X-ray, such as mild-to-severe multifocal soft tissue opacities (seen as ground-glass opacities described in the CT scans). Pleural effusions were also seen.
Necropsy showed that the virus was detectable in almost 100% of lung samples, at a mean of 4-6 log copies/100 mg of lung tissue in each lobe. This indicates that viral RNA increases by 4 logs from 1-2 days after infection, proving that the virus undergoes early and massive replication in macaques.
The lungs showed interstitial and alveolar pneumonia and were the organs most severely affected by the disease. Fluorescence immunohistochemical analysis showed the viral antigens to be present in the lungs and tonsils, with higher ACE2 expression in virus-exposed vs. naïve animals.
The cytokine profile showed an early massive response to viral infection, with an increase in IL-12p4, IL-18, TNF, and IL-1Ra over time. The rise in Type I IFN-a and IL-6 could cause the so-called “cytokine storm” that is closely linked to acute respiratory distress syndrome (ARDS) if it occurs in an unregulated manner.
In short, acute infection occurs following exposure to SARS-CoV-2 in macaques, causing pneumonia and early antiviral response.
The Progression Study
The next step was to understand how the infection progresses over time and with age. The researchers used six young and six old macaques, and followed them up for 14-17 days, along with 4 control macaques. To compare how the infection progressed in other NHP, they also infected 6 baboons and 6 marmosets.
The researchers found that the acute signs of infection and disease improved over time, with no age-dependent variation. 3/12 animals showed a persistent rise in serum CRP after the third day of infection, and all showed metabolic impairment throughout the two weeks of the study period. Red blood cells fell and rose to normal again by the 9th day, while neutrophils in peripheral blood stayed unchanged through days 3-14. Weight loss was seen in both old and young animals.
Most of the macaques had detectable viral RNA in BAL, but at very low copy numbers. The nasal swabs tested positive for the viral RNA in half the macaques at 3 days, at 10/12 animals at the 9th day and half by the end of the study period, which indicates viral persistence in the respiratory tract for two weeks or more in clinically convalescent animals.
Viral RNA levels dropped compared to the early-phase study, by the end of the study period. Most animals had detectable viral RNA in the lung tissue. These results indicate that clinical recovery occurs but not sterilizing immunity.
Comparisons Between Species
In the baboons, the early detection pattern was similar to that of macaques, but viral RNA persisted in baboons over the long term to a greater extent than with macaques. Here too, the lungs were the most severely and commonly affected, with prominent mononuclear inflammation in all animals.
The infection appeared milder in marmosets, with less than 4 logs of viral RNA detectable in nasal swabs on the 3rd day, but none at or after the 6th day. Pneumonic changes were also less frequent in these animals.
CT scans showed moderate progressive pneumonia in all macaques, but more in old than in young animals, which resolved by the 12th day, along with low lung and nasal viral loads. Baboon lungs are most severely affected, with more significant viral shedding as well as a persistent virus in the respiratory compartment.
Implications for Future Therapeutic Development
In short, the studies show that “three genera of NHPs develop different degrees of COVID-19 following SARS-CoV-2 infection when evaluated side by side, with baboons exhibiting moderate to severe pathology, macaques exhibiting moderate pathology and marmosets exhibiting mild pathology. Viral RNA levels in BAL, NS, and lungs are consistent with the levels of pathology.” This provides a quantifiable metric for the accurate evaluation of vaccines and therapies.
The study also demonstrated that cone beam CT scanning could be used alongside innovative algorithms to quantify the degree of lung involvement.
Secondly, they demonstrate the recruitment of specific myeloid series into the lung tissue, especially of the monocyte, neutrophil, and dendritic cell series, all containing detectable viral protein. The stimulus for these migrations is probably the virally-induced ramping up of bone marrow production of these cells. The high level of expression of the type 1 IFN response as well as other pro-inflammatory cytokines may explain why pneumonia first develops and is then controlled by the immune response in most animal hosts.
Finally, the lack of age-related disparity in severity of infection may suggest that coexisting illness rather than age per se is responsible for the higher infection rate and mortality in older and sicker humans. Again, the relative susceptibility of the baboons to COVID-19 disease may help explore this area in humans with comorbidities like diabetes, cardiovascular disease, and who are elderly.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Singh, D. K., et al. (2020). SARS-CoV-2 Infection Leads to Acute Infection with Dynamic Cellular and Inflammatory Flux in The Lung That Varies Across Nonhuman Primate Species. bioRxiv preprint. doi: https://doi.org/10.1101/2020.06.05.136481. https://www.biorxiv.org/content/10.1101/2020.06.05.136481v1
- Peer reviewed and published scientific report.
Singh, Dhiraj Kumar, Bindu Singh, Shashank R. Ganatra, Michal Gazi, Journey Cole, Rajesh Thippeshappa, Kendra J. Alfson, et al. 2021. “Responses to Acute Infection with SARS-CoV-2 in the Lungs of Rhesus Macaques, Baboons and Marmosets.” Nature Microbiology 6 (1): 73–86. https://doi.org/10.1038/s41564-020-00841-4. https://www.nature.com/articles/s41564-020-00841-4.