The COVID-19 pandemic is affecting millions of people around the world and has taken a toll of over 411,000 lives. Yet after five months, there are immense gaps in our knowledge as to the factors that increase or inhibit viral transmission.
Initially, scientists attempted to invoke meteorological factors to explain the spread of the SARS-CoV-2 in mainly cold climates, which were experiencing winter. However, factors like temperature, relative humidity, and exposure to natural ultraviolet radiation from sunlight, do not explain the variation in disease incidence fully. Now, a new study published on the preprint server medRxiv* in June 2020 uses certain observations to build a hypothesis as to the role played by pollen in the seasonal waxing and waning of flu-like epidemics, including COVID-19.
Pollen and Influenza
Pollen is known to be an antiviral substance, and also has anti-influenza and allergenic effects. It is also known to activate the immune system. Dutch researchers identified pollen as one of the factors that independently act to reduce the incidence of flu-like epidemics over the period 2016 to 2019 in the Netherlands.

Bee covered with yellow pollen, collecting nectar in flower. Image Credit: Ihor Hvozdetskyi / Shutterstock
The current study is based on the finding that pollen and flu seasons are consistently and predictably found to follow each other each year in countries within a temperate climate zone, which cannot be explained by purely meteorological factors. The beginning and ending of moderate flu-like epidemics and of the current COVID-19 pandemic is also found to mirror the points in time when allergenic pollen grain release crosses a threshold of about 100 grains/m3 per week.
Earlier research has shown that cold, flu and similar illnesses circulate in fall and winter in the Northern Hemisphere, but leave in May. The opposite pattern prevails in the Southern Hemisphere during this period. Every new pandemic of flu-like illness since 1889 has emerged towards the end of the flu season of that year, including the current COVID-19 pandemic. An earlier study showed that most such pandemics also occur in multiple waves, with the first one typically being short-lived. This carries the implication that COVID-19 will also repeat itself in multiple seasonal waves.
Ultraviolet Radiation, Pollen and FLI
The ultraviolet light theory which attributes the onset of flu-like illnesses (FLI) to a lack of ultraviolet light in winter and fall, with the consequent lack of its viral activity and lower immune activation, does not explain why the flu season begins in early August, at the hottest and sunniest time of the year, in the Netherlands. Moreover, high ultraviolet and temperature conditions do not explain the decline of the current COVID-19.
What then, do these factors explain? The researchers note that these are associated with pollen ripening and dispersion. With this in mind, the researchers put forward the hypothesis that pollen bio-aerosols affect the incidence of FLI and of COVID-19.
The Study: Examining Pollen, Weather, and FLI
The researchers examined the following parameters: the weekly allergenic, non-allergenic, and total pollen counts in grains/m3; the weekly incidence of flu-like illness; and meteorological data include daily relative humidity, average temperature, and solar radiation.
The hay fever index, defined as the total turnover for hay fever medication, is also used to test the use of allergenic vs. non-allergenic pollen grains in this scenario. All the parameters were followed over 42 weeks, from the first week of 2016 to the 18th week of 2020, so as to include the COVID-19 pandemic, except for the hay fever index for which data was available only until week 10 of 2019.
The weekly change in flu incidence was calculated to measure the progression of the FLI lifecycle, with a decline taken to mean R0<1 and an increase, meaning R0>1. R0 is the reproduction number for these viruses. Three weeks moving average (3WMA), which includes two forward-looking weeks, was used to include both changes in the incidence of such diseases as well as the incubation period of about two weeks.
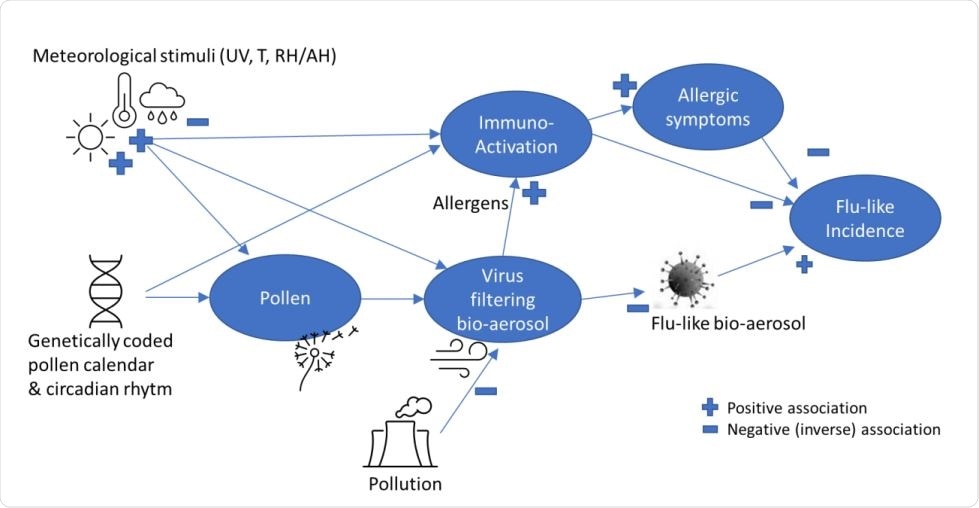
A simplified theoretic model explaining pollen-flu inverse seasonality, whereby pollen might have a direct (I) “anti-viral”, indirect allergenic (II) and/or immune triggering (III) function, inhibiting flu-like epidemic incidence in combination with meteorological conditions and triggers.
Pollen Bursts Precede Declines in FLI
The researchers found that pollen grain release was, on average, 732 grains/m3 per week, with allergenic grains at 349 grains/m3, non-allergenic at 383 grains/m3, and 47 consults/100,000 citizens/week for FLI. Pollen bursts were continuous, but only a few were allergenic pollen bursts. However, such pollen bursts were found to precede each decline of FLI consults.
Earlier work by the same researchers showed a significant inverse relationship between allergenic pollen release and changes in FLI incidence, but not with FLI incidence per se because pollen bursts are typically short and intense. The current study looked at total pollen counts instead of only allergenic pollen, showing highly significant inverse correlations with FLI.
When the data is adjusted for the two weeks of incubation, the inverse correlation becomes even stronger. Thus, pollen per se is related with respect to time with FLI incidence. Moreover, the pattern of decline in FLI consults beginning after the first bursts of pollen release and showing a sharp increase after pollen counts approach zero indicate a causal role for pollen. The first wave of COVID-19 fits this pattern as well.
The researchers say, “These inverse correlations provide thus further support for the alternative hypothesis that the presence of an elevated level of pollen has an inhibiting effect on flu-like incidence, and starts to immediately influence the direction and course of the epidemic life cycle. COVID-19 behaves according to the expected pollen-flu seasonality like all other flu-like pandemics have since the end of the 19th century.”
The use of the 3WMA strengthens these correlations still more, for both allergenic and total pollen counts, especially after adjusting for the incubation period and with the inclusion of the 2019-2020 flu season as well. These findings lend support to the relationship of COVID-19 with pollen-induced seasonality of FLI.
Simple linear regression analysis shows a very significant decline of FLI incidence, again indicating that total pollen counts are a predictor of FLI seasonality. The positive effect of total pollen on hay fever incidence and the negative effect on FLI incidence further strengthens the inverse association between total pollen and FLI.
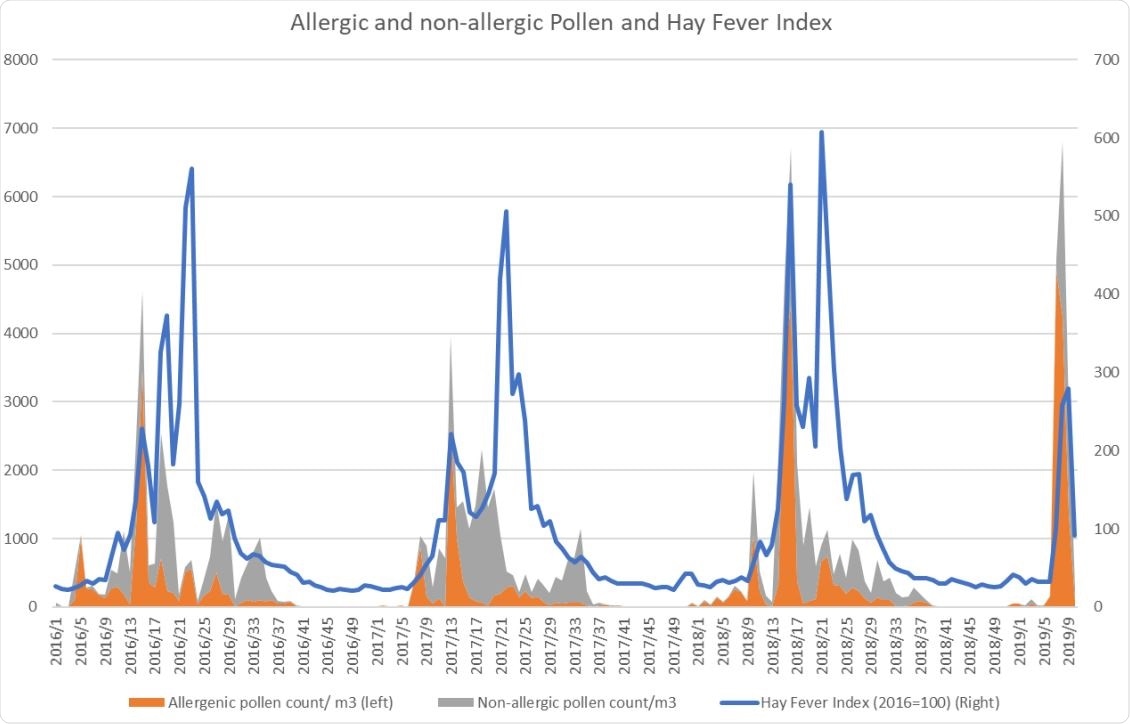
Both allergenic and non-allergenic pollen are associated with hay fever
Weather Conditions Inhibit FLI Via Pollen and Immune Activation
How then do relative humidity, temperature, and solar radiation fit into this picture? The release of pollen increases with warm, sunny, and dry weather. The relationship with temperature may be significant only towards the beginning of the pollen season as it shifts the pollen calendar forward. Thus, the temperature probably has no direct effect on FLI-causing aerosol viruses or the lifecycle of the epidemic, nor does it predict the end of the flu season.
Relative humidity surprisingly increases the incidence of FLI in the Netherlands, probably because rain reduces pollen dispersal. Sunlight, however, has a very marked inverse association with changes in FLI incidence, which could mean that sunlight not only promotes pollen release and activates the immune system via the melatonin system, but could destroy aerosol viruses before they can infect other hosts.
A New Pollen-Sunlight-FLI Model
The researchers then developed a new model based on changes in FLI incidence, solar radiation threshold, total pollen, and allergenic pollen. They found that the highest inverse correlation of FLI was with a solar radiation threshold of 510 J/cm2, allergenic pollen at 120 pollen grains/m3 per week, and total pollen at 610 pollen grains/m3 per week.
They observed the past years, finding that these pollen thresholds were crossed in week 10 (± 5 weeks) and week 33 ((± 2 weeks) each year, which corresponds to the peak of the FLI epidemic and the start of the new flu season, respectively.
The researchers explain this finding thus: “This finding is in line with our virus filtering aerosol hypothesis in which aerosol pollen de-activate aerosol viruses before they can infect a new host. However, as so-called non-allergenic pollen also contributes to the incidence of hay fever in our study, another explanation might be that non-allergenic pollen have immuno-activating effects as well.”
As for the inverse relationship of hay fever with FLI incidence, the explanations include:
- Allergic symptoms may hinder infection with flu-like viruses which cannot reach the susceptible lung cells
- Hay fever medication reduces false positives for FLI by suppressing symptoms of cold as well as, possibly, symptoms of FLI as well.
This model could thus explain how FLI incidence is related to the seasons, and allow reliable prediction of onset and end dates. It can also explain the effect of pollen, solar radiation, and humidity on FLI, as well as the emergence of the COVID-19 towards the end of the flu season and in the Northern Hemisphere which is much more crowded than the Southern Hemisphere.
Implications for COVID-19 Management
The study concludes: “A consequence of our findings could potentially be that social distancing and other preventive behavior are especially important during the flu-like season, but probably less relevant during pollen season when nature takes care by inhibiting viruses.”
Further work is required to understand how aerosol pollen affects such viruses, whether pollen indeed activates the immune system to deal with such viruses, and the mechanism of immune activation if present. These findings could help develop new therapies.
Importantly, the study could help conclude that the current pandemic of COVID-19 is seasonal, and multi-cyclic, and will, therefore, return around week 33 as with other FLI viruses, following the end of pollen season. This will mandate preparation for social distancing and other measures during the flu season until other means are available to inhibit viral spread.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources