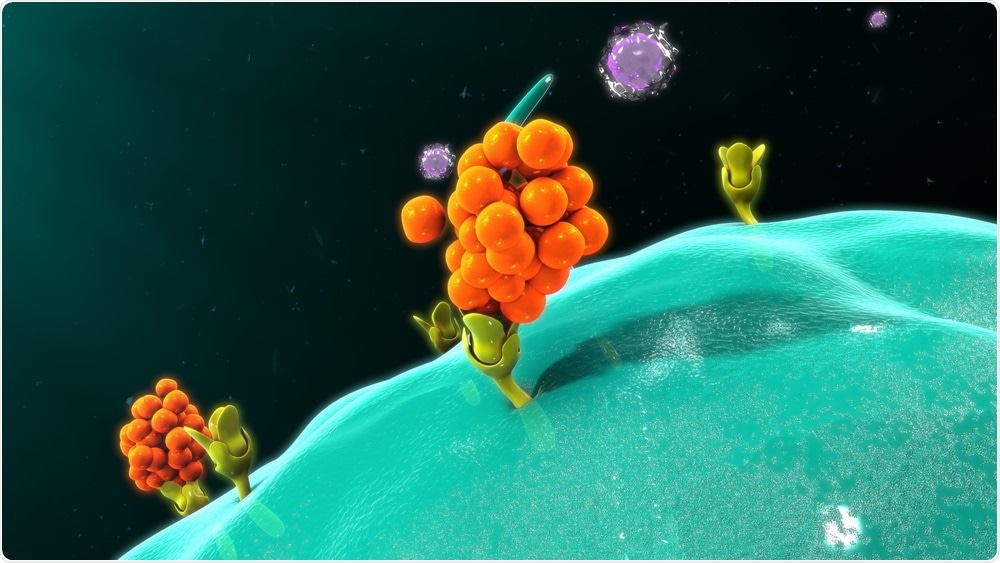
Macrophage releasing cytokines. Image Credit: sciencepics / Shutterstock
An ongoing COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), had a severe impact not only on human health, but also on health care systems, society, and the global economy. Although most people do not develop severe forms of the disease, it can manifest with grave respiratory problems and death.
In the short period since disease emergence, many studies have described abnormal levels of various cytokines and chemokines (i.e., small cell-signaling proteins) due to SARS-CoV-2 infection. The underlying mechanism is the depletion of antiviral defenses linked to the innate immune response, as well as increased production of pro-inflammatory cytokines.
This can subsequently result in the so-called 'cytokine storm' – an uncontrolled overproduction of inflammation markers that prompt and maintain an aberrant systemic inflammatory response, which leads to acute respiratory distress syndrome (ARDS) and, often, a lethal outcome.
Researchers from the University of Granada, the Institute of Biosanitary Research in Granada, as well as from the University Hospital Virgen de las Nieves in Granada, Spain, conducted a thorough review in other to pinpoint exact molecular changes that can be linked to SARS-CoV-2 infection and the severity of the disease.
.jpg)
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (pink) heavily infected with SARS-COV-2 virus particles (green), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Elevated levels of interleukins
SARS-CoV-2 appears to activate and prompt the maturation of interleukin-1β, which in turn activates other pro-inflammatory cytokines – most notably interleukin-6 and tumor necrosis factor-alpha (TNF-α). Consequently, interleukin-1β is partly responsible for cytokine storm prompted by this virus and other coronaviruses.
Elevated levels of either interleukin-2 or its receptor have been observed in patients with COVID-19, and different research reports state that such increase is directly proportional to disease severity. The same is valid for interleukin-4 and interleukin-6, which are both related to cytokine storm and poor COVID-19 prognosis.
"With regard to the important role of interleukin-6 in the SARS-CoV-2-induced cytokine storm and its evasion, it has been reported that the monoclonal antibody tocilizumab acts by blocking the receptor of interleukin-6 and has been reported to reverse cytokine hyperproduction, inflammation, and pulmonary fibrosis", further explain study authors.
When interleukin-10 is concerned, its values are also increased in COVID-19 patients. At the same time, certain authors indicate that this cytokine may be hyper-expressed in anti-SARS-CoV-2 immunity, especially in the elderly concerning a 'hyperinflammatory response' (potentially related to the reduction of T-cell receptors).
In addition, elevated levels of interleukin-12, interleukin-13, interleukin-17 have also been observed in COVID-19 patients, correlating well with the viral load in the human organism. The common notion is their propensity to induce inflammation.
Other cytokines and biomolecules
Significantly elevated levels of macrophage colony-stimulating factor in patients with COVID-19 have been observed, while its hyperexpression was linked to the severity of lung damage, which may aid in predicting disease course. Similar has been observed for granulocyte and granulocyte-macrophage colony-stimulating factors.
Furthermore, elevated levels of interferon-gamma-inducible protein-10 (IP-10) have been observed in a myriad of (mostly viral) infections. "Serum IP-10 levels were found to be elevated in patients with COVID-19 and even higher in those who required ICU admission, suggesting their relationship with lung damage and disease severity", say study authors.
Tumor necrosis factor α (TNF-α) was among cytokines whose overproduction was linked to a poor prognosis in patients with original SARS and MERS. Likewise, it was noted that its levels also correlate with the disease severity in COVID-19 patients, which is the reason why anti-TNF-α antibodies were considered as a potential treatment approach.
Most of the literature had shown that interferon-γ levels were higher in patients infected with SARS-CoV-2 when compared to healthy individuals. Still, this specific cytokine could not be used as a specific marker to differentiate those who need intensive care.
Besides cytokines, other biomolecules have shown increased expression in patients with COVID-19, including growth factors. Among them, vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF) are found to be elevated in COVID-19 patients, especially those necessitating ICU admission.
Using cytokines to forecast the course of COVID-19
"Findings on the role of cytokine storm associated with SARS-CoV-2 infection can be useful in order to manage this highly virulent disease", emphasize study authors in their paper.
However, there is still not a single cytokine marker that can be used to predict the further course of COVID-19, which means we may need to utilize a combination of markers to differentiate between different clinical presentations.
What this study shows is that we can be quite certain that the immunological reaction triggered by SARS-CoV-2 infection mobilizes a panoply of cytokines, mainly of pro-inflammatory nature. Consequently, the inhibition of their activity is definitely a viable therapeutic strategy.