
Study: Time is of the essence: containment of the SARS-CoV-2 epidemic in Switzerland from February to May 2020. Image Credit: Roger Gantner / Shutterstock
The first case in this country came from a region adjoining an affected region of Italy, but the disease rapidly spread over the small nation. In response to the outbreak, a sequence of non-pharmaceutical interventions (NPIs) was rapidly introduced, including the closure of primary schools, stores selling non-essential goods, and restaurants, as well as limiting the gathering of over five people on March 20, 2020.
The epidemic showed a decline after the introduction of these measures in March. By May 10, 2020, the restrictions were lifted. The paper by researchers at the University of Bern is aimed at showing how the time of implementation of NPIs affects the course of the epidemic and its outcome.
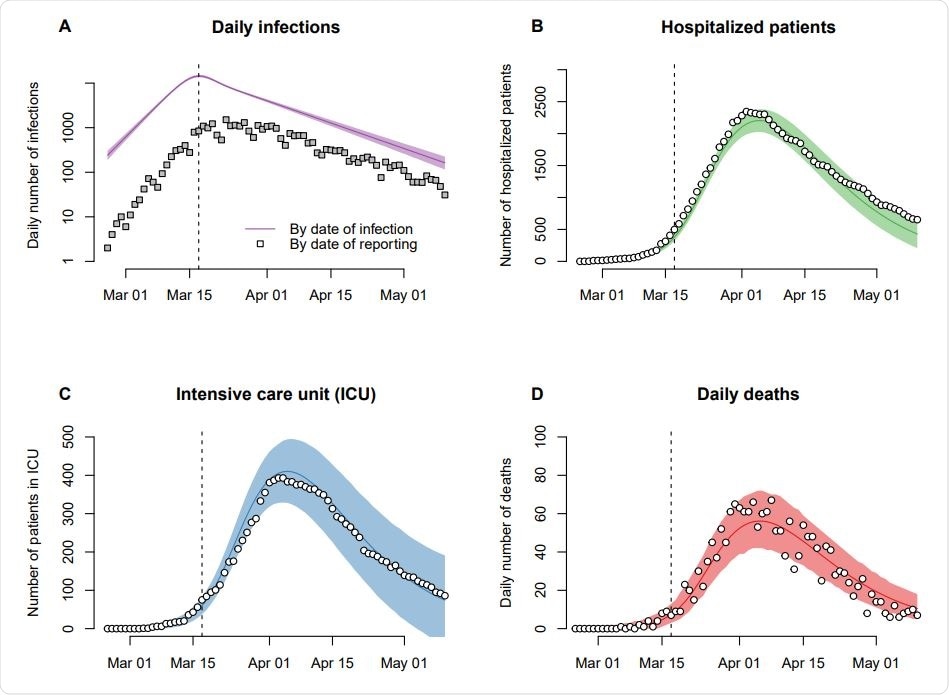
Modeled number of new infections, hospitalized patients, intensive care unit (ICU) occupancy, and deaths during the SARS-CoV-2 epidemic in Switzerland. The solid lines show the maximum likelihood estimate of the model and the shaded areas correspond to the 95% prediction intervals. The model was fitted to the data shown as white circles. Reported number of infections (gray squares) are shown for comparison. The vertical dashed line indicates the strengthening of social distancing on 17 March 2020.
Potential Effects of Earlier or Later NPIs
The researchers used modeling to estimate the effect of different scenarios on the Swiss epidemic. Namely, if the NPIs had been put in place a week earlier or a week later, how would the infection incidence, the number of hospitalized cases, and the mortality, have changed?
The research was based on population-based transmission models and included the stepwise introduction of NPIs. Earlier research showed that these led to a steep reduction of the effective reproduction number (Re) in Switzerland.
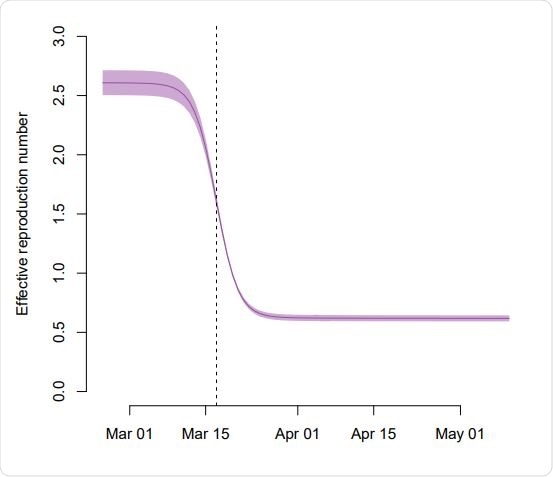
Reduction of the effective reproduction number Re during the SARS-CoV-2 epidemic in Switzerland. The solid line shows the maximum likelihood estimate of the model and the shaded area corresponds to the 95% compatibility interval. We assumed that the sequential introduction of NPIs resulted in a sigmoid reduction of the transmission rate over a period of around 2 weeks. The vertical dashed line indicates the strengthening of social distancing on 17 March 2020.
Using public data on the daily number of confirmed cases, hospitalizations, intensive care unit (ICU) admissions, and deaths related to the virus, the researchers found that initially, the infections went up exponentially.
The researchers also estimated that the total number of infections was about tenfold the number of diagnosed and confirmed cases initially. Later, the diagnosed cases amounted to about 20% of the total, but finally, after all NPIs were in place, fell again to about 10% of the total. The estimated total, therefore, amounted to about 264,000 cases.
Using simulations of earlier introduction of NPIs, the model showed that about 2,000 deaths would have occurred if NPIs continued to affect the number of deaths after May 10 negatively. If they had been implemented a week earlier, the model concludes that the peak number of hospitalizations would have been much lower, at ~ 440, as would have been the peak ICU occupancy and mortality, at ~88 and 400 respectively.
If NPIs had been introduced a week later, these numbers would have gone up substantially, with a peak hospitalization number of about 10,200, peak ICU occupancy of 1,900, and mortality of over 8,000, respectively.
Doubling Time Triples with NPIs
The current study showed that the effective reproduction number (Re) fell from about 2.6 at the beginning to 0.64, which corresponds to a doubling time of about 3 days and 9 days at the beginning of the epidemic and the post-lockdown phase, respectively. This underlines the urgency of early NPIs in containing the spread of the virus.
The researchers comment, “One week of exponential increase in new infections during the early epidemic spread required 3.1 weeks of ‘lockdown’ to reduce the number of infections to the same level.”
Implications of the Study
This is the first study to analyze the possible effects of counterfactual scenarios concerning alterations in the timing of NPI implementations. The findings are partly supported by the lower mortality in Austria, which reported its first few cases at the same time as Switzerland, and which was also the victim of spread from adjoining Lombardy, in Italy. However, the early and strict introduction of NPIs within a week of the first case led to a reduced number of deaths.
Moreover, the researchers point out that the high peak ICU occupancy rate of almost 2,000 that could potentially have resulted from a single week’s delay in NPIs would probably have overwhelmed the national healthcare system, since the effective capacity of ICUs in Switzerland was only about 1,275 in April 2020.
In short, the study concludes, “Our study illustrates that time is of the essence when it comes to outbreak response. We showed that while an earlier implementation of NPIs in Switzerland would have resulted in considerably lower numbers of hospitalized cases and deaths, the measures that were taken successfully prevented a much higher burden of SARS-CoV-2-related morbidity and mortality.”
Since one week of exponential virus spread requires three weeks of lockdown to bring the number of daily cases back to the original level again, delay not only boosts the number of deaths but prolongs the period of lockdown. An earlier imposition of strict NPIs would, therefore, reduce the social and economic burden of these measures. Secondly, there are significant differences in the number of infections in different cantons, and this may indicate that new local outbreaks are probably going to be confined to separate regions.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.