A study conducted by researchers at the University of California, Los Angeles and Cedars Sinai Medical Center suggests that smoking increases the risk of more severe lung disease in cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
The team found that exposure to cigarette smoke increased the number of infected and apoptotic cells in the airway and that SARS-CoV-2 prevented the usual repair response to airway injury.
The study also suggested that modulation of the interferon response by SARS-CoV-2 could be linked to the increased number of infected cells on exposure to cigarette smoke.
“Consistent with this hypothesis, we found that the smoke-induced increase in SARS-COV-2 infection could be abrogated by treatment with exogenous interferonβ-1,” writes the team.
Brigitte Gomperts and colleagues say it is not yet clear whether former smokers are at a similar increased risk of more severe infection and that this still needs to be investigated.
Overall, the study provides evidence that aggressive measures are needed to stop smoking and lower the risk of more severe coronavirus disease 2019 (COVID-19), say the researchers.
A pre-print version of the paper is available on the bioRxiv* server, while the article undergoes peer review.
Researchers suspect smoking is a significant risk factor for severe COVID-19
SARS-CoV-2, the causative agent of the COVID-19, infects cells by binding to the angiotensin-converting enzyme 2 (ACE2) receptor present on host cells. The infection is primarily a respiratory illness, and ACE2 is highly expressed in ciliated cells of the upper airways.
Smoking, which is a leading cause of chronic lung disease, has previously been shown to decrease innate mucosal immunity and increase viral replication. Reported mechanisms include degradation of the type 1 interferon receptor and reduced airway immunity through inhibition of type II interferon-dependent gene expression.
Given that smoking is a common cause of chronic lung conditions, researchers have suggested that it may be an important risk factor for severe COVID-19.
“Accordingly, the World Health Organization reviewed the available evidence and concluded that smoking is associated with increased severity of disease and death in hospitalized COVID-19 patients, although they could not quantify the risk to smokers,” said Gomperts and colleagues.
However, the majority of demographic studies are now linking current smoking to an increased risk for more severe disease and death.
Still, no studies have assessed the effects of smoke exposure on the airway epithelium in cases of SARS-CoV-2 infection, and many questions remain about whether smoking influences the infection of airway cells.
What did the researchers do?
Gomperts and team exposed mucociliary epithelial air-liquid interface (ALI) cultures derived from the airway basal stem cells (ABSCs) of human non-smokers to cigarette smoke and then infected them with SARS-CoV-2.
Following exposure to cigarette smoke, there was a higher number of infected airway cells, as well as a higher number of apoptotic cells. Acute cigarette smoke exposure also resulted in airway injury that triggered the proliferation of ABSCs to repair the airway.
On the other hand, infecting the ALI cultures with SARS-CoV-2 – either alone or in combination with cigarette smoke exposure – stopped the proliferation of ABSCs and prevented the usual airway repair response.
Cigarette smoke reduced the interferon response
Next, the team used single-cell profiling to explore why the ALI cultures may be more susceptible to the virus following cigarette smoke exposure.
This revealed that SARS-CoV-2 decreased the expression of many host genes across all types of airway cells.
However, interestingly, the virus-induced the expression of interferon response genes, but only when this was not combined with cigarette smoke exposure. The combination of SARS-CoV-2 infection and smoke exposure reduced the interferon response.
“Cigarette smoke exposure reduces the interferon response, suggesting that the modulation of the interferon response by SARS-COV-2 is causally linked to higher infection in smoke-exposed cultures,” writes the team.
Consistent with this hypothesis, the researchers found that treating the smoke-exposed ALI cultures with exogenous interferonβ-1 abrogated SARS-CoV-2 infection.
The findings have important implications for smokers
The researcher say the findings have important implications for the severity and spread of disease among people exposed to cigarette smoke.
“The increased number of infected cells in smokers has implications for more severe infection in smokers resulting in increased lung disease,” say Gomperts and colleagues.
“Overall, our data provide evidence for the need for aggressive health measures to stop smoking to reduce severe COVID-19,” they conclude.
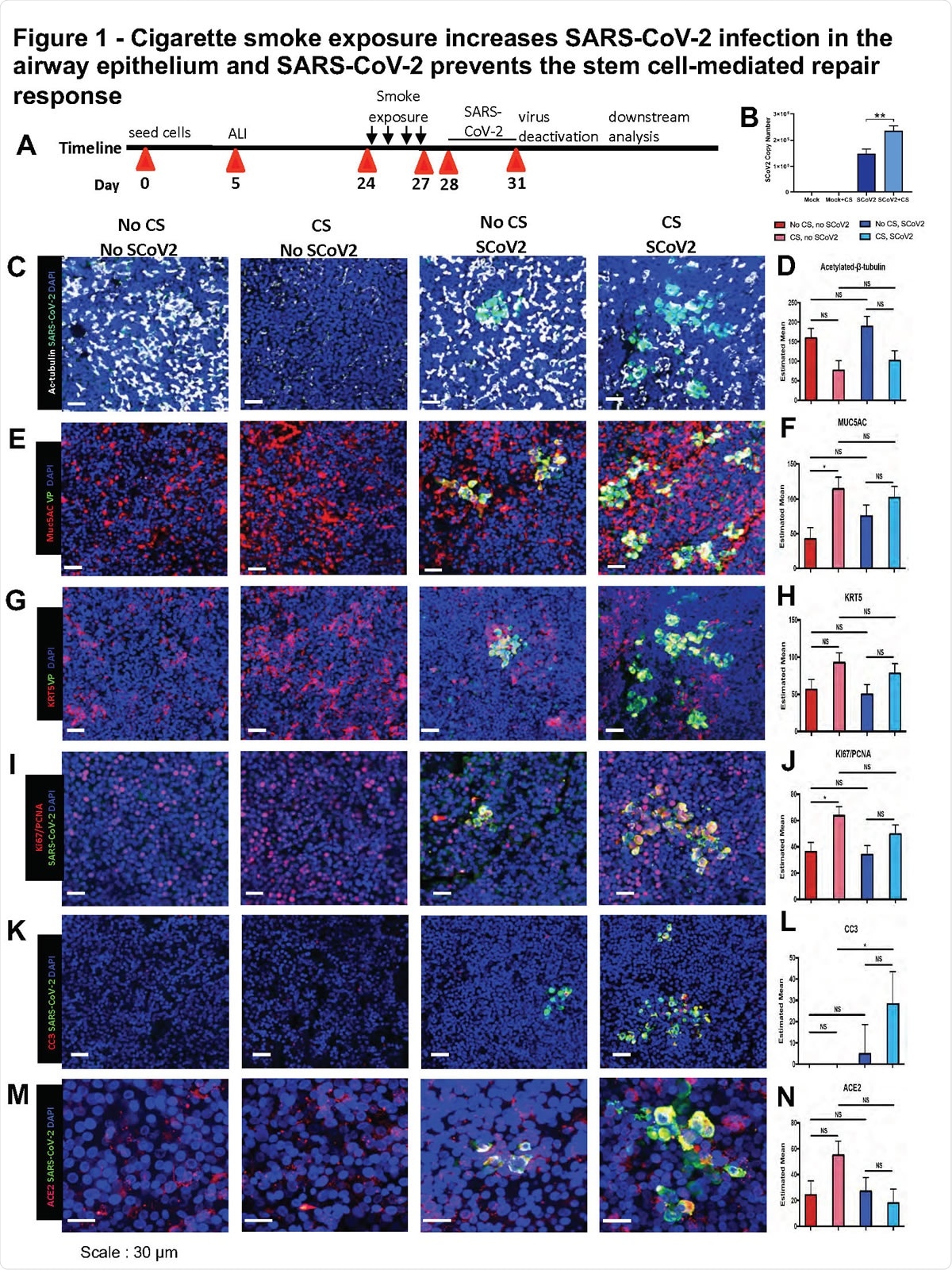
Cigarette smoke exposure increases SARS-CoV-2 infection in the airway epithelium A. Experimental schematic outline showing the total days in culture with days of experimental manipulations B. Quantification of SARS-CoV2 viral load with and without smoking exposure by quantitative real-time PCR of viral mRNA C. IF images of ciliated cells (white) and SARS-CoV-2 (green) infected cells in ALI cultures across the four exposure conditions of no smoking and no virus, smoking and no virus, no smoking and virus and both smoking and virus exposures D. Quantification of number of ciliated cells across the four exposure groups E. IF images of Muc5AC (red) mucus cells and SARS-CoV-2 (green) infected cells in ALI cultures across the four exposure conditions F. Quantification of number of Muc5AC+ mucus cells across the four exposure groups G. IF images of K5 (red) ABSCs and SARS-CoV-2 (green) in ALI cultures across the four exposure conditions H. Quantification of number of ABSCs across the four exposure groups I. IF images of ACE2 (red) and SARS-CoV-2 (green) in ALI cultures across the four exposure conditions J. Quantification of number of ACE2+ cells across the four exposure groups K. IF images of both Ki67 and PCNA (red) and SARS-CoV-2 (green) expressing cells in ALI cultures across the four exposure conditions L. Quantification of number of proliferating cells across the four exposure groups M. IF images of cleaved caspase 3 (CC3)(white) and SARS-CoV-2 (green) for apoptosis across the four exposure conditions N. Quantification of number of apoptotic cells across the four exposure groups Bar graph represents SEM, n = 3-6. *p < 0.05, ** p<0.01, ns = not significant by Turkey test.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Gomperts B, et al. Direct exposure to SARS-CoV-2 and cigarette smoke increases infection severity and alters the stem cell-derived airway repair response. bioRxiv, 2020. doi: https://doi.org/10.1101/2020.07.28.226092
- Peer reviewed and published scientific report.
Purkayastha, Arunima, Chandani Sen, Gustavo Garcia, Justin Langerman, David W. Shia, Luisa K. Meneses, Preethi Vijayaraj, et al. 2020. “Direct Exposure to SARS-CoV-2 and Cigarette Smoke Increases Infection Severity and Alters the Stem Cell-Derived Airway Repair Response.” Cell Stem Cell 27 (6): 869-875.e4. https://doi.org/10.1016/j.stem.2020.11.010. https://www.cell.com/cell-stem-cell/fulltext/S1934-5909(20)30548-8.