Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily targets epithelial cells on mucosal surfaces. Secretory Immunoglobulin A (IgA), found on mucosal surfaces, plays a very crucial role in fighting against pathogens targeting these surfaces. Individuals who suffer from milder forms of SARS-CoV-2 infection generally have variable and low serum neutralizing antibody responses. Though it is known that potent Immunoglobulin G (IgG) antibodies are capable of neutralizing the virus, not much is known about secretory antibodies like IgA that could control the initial transmission from the mucosa.
.jpg)
Colorized scanning electron micrograph of a cell (blue) heavily infected with SARS-CoV-2 virus particles (red), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Mechanism of SARS-CoV-2 infection
SARS-CoV-2 has a trimeric spike surface protein (S) that mediates its entry into host cells. Initially, the virus infects the epithelial cells of the nasopharynx. During this initial stage, the receptor-binding domain (RBD) of the surface protein S interacts with the angiotensin-converting enzyme-2 (ACE-2) receptor. Subsequently, the virus spreads to other epithelial cells and starts expressing ACE-2 in the lung and the gut. These lung and gut tissues are rich in nasopharynx-associated and gut-associated lymphoid cells. That must be why inhaled vaccines that specifically target these tissues seem to be more effective in fighting against SARS-CoV-2.
Although nasopharynx-associated and gut-associated lymphoid tissues produce vast quantities of IgA antibodies, they exist as monomers in circulation. However, IgAs found in secretions exist mostly in the dimeric form, and they are also found in higher concentrations.
Even though most infected individuals produce antibodies in response to the SARS-CoV-2 virus, the neutralizing response varies a lot, and about 30% of the patients show neutralizing activity below 1:50 in pseudovirus assays. Neutralization is usually linked to RBD binding activity measured by ELISA and prolonged infection.
Experiments that cloned IgG antibody from recovered individuals showed that neutralizing antibodies target many distinct non-overlapping epitopes on the RBD. Some of these antibodies are very powerful and can prevent or treat SARS-CoV-2 infection in animal models.
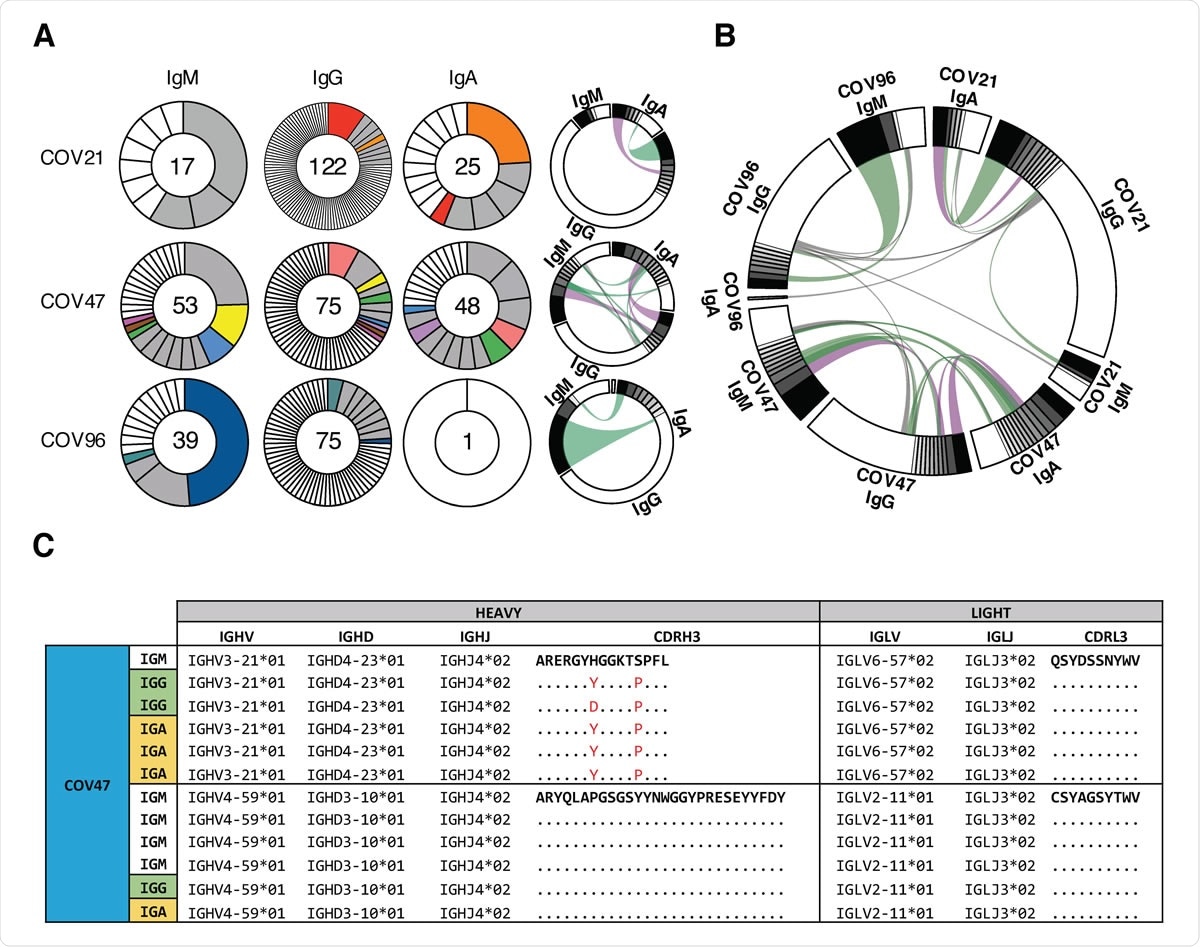
Plasma IgA against SARS-CoV-2 RBD. (A) ELISAs measuring plasma IgA reactivity to RBD. Graph shows optical density units at 450 nm (OD, Y axis) and reciprocal plasma dilutions (X axis). Negative controls in black; individuals 21, 47, 96 in blue, red and green lines and arrowheads, respectively (11). (B) Graph shows normalized area under the curve (AUC) for 8 controls and each of 149 individuals in the cohort. Horizontal bar indicates mean values. Black dots indicate the individuals that are 2 STDV over the mean of controls. (C) Subjective Symptom (Sx) severity (X axis) is plotted against the normalized AUC for IgA binding to RBD (Y axis). r= 0.3709, P < 0.0001. (D) Normalized AUC of anti-RBD IgA ELISA for males (n=83) and females (n=66); P =0.0016. (E) Normalized AUC of anti-RBD IgA ELISA for outpatients (n=138) and hospitalized (n=11) individuals; P = 0.0035. (F) Normalized AUC of anti-RBD IgA ELISA for patients with gastrointestinal (GI) symptoms (n=32) and without GI symptoms (n=117); P = 0.0030. The r and P values for the correlations in (C) were determined by two344 tailed Spearman’s. For (D-F) horizontal bars indicate median values. Statistical significance was determined using two-tailed Mann-Whitney U test.
IgA Response to SARS-CoV-2
IgA antibodies are produced rapidly right after SARS-CoV-2 infection, and their levels remain elevated in plasma for about 40 days after symptom onset. Though we know that IgA antibodies can bind to the RBD and neutralize SARS-CoV-2, the molecular nature of the IgA response to the virus has not been reported before.
This new study analyzed 149 convalescent individuals who showed measurable IgA neutralizing responses to the SARS-CoV-2 virus. To study IgA’s contribution to the anti-SARS-CoV-2 RBD response, the researchers tested plasma samples for RBD binding using ELISA. A positive control sample (COV-21) was also used for normalization of the area under the curve (AUC). Eight samples from independent, healthy donors served as negative controls.
The team found that 78% and 15% of the individuals who participated in the study showed IgG and IgM anti-RBD levels that were at least 2 SDs above control, and only 33% of the individuals had the same results for IgA. So, in individuals examined about 40 days after infection, the circulating anti-RBD IgA levels are higher than IgM and lesser than IgG.
They also observed that while females had lower IgA levels than males, there was no age-related correlation. Also, individuals who suffered from gastrointestinal symptoms showed significantly higher plasma levels of anti-RBD IgA than IgG. The researchers also found that dimeric IgA is more potent against SARS-CoV-2 than monomeric IgA.
What did the researchers conclude?
The study results clearly showed that serum IgA responses to SARS-CoV-2 correlate with IgG responses. Monomeric IgA is about 2-fold less potent than IgG, and dimeric secretory IgA present in the mucosa is much more effective compared to the monomeric form. This makes dimeric IgA a far more strong neutralizer than IgG.
“On average, there was a 15-fold geometric mean increase in activity for the dimer over the monomer against SARS-CoV-2 and less variability in the degree of enhancement in microneutralization compared to pseudovirus assays”, say the authors.
The increased potency of dimeric IgA shows that crosslinking the S protein on the viral surface increases neutralization through increased affinity. Although it is still not clear if this effect is due to inter- or intra-spike crosslinking, it surely indicates that increasing the valency of antibodies or drugs that block viral entry through RBD binding could make them more potent.
At a time when scientists all over the world are racing against time and experimenting with several different candidate vaccines to SARS-CoV-2, these findings about secretory IgA responses may be particularly vital, more so because potent dimeric forms of IgA are found in the mucosal surface which is the entry point of SARS-CoV-2 virus. Thus, the study reveals that vaccines specifically designed to trigger mucosal IgA responses may prove to be particularly effective in preventing SARS-CoV-2 infection.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Enhanced SARS-CoV-2 Neutralization by Secretory IgA in vitro Zijun Wang, Julio C C Lorenzi, Frauke Muecksch, Shlomo Finkin, Charlotte Viant, Christian Gaebler, Melissa Cipolla, Hans-Heinrich Hoffman, Thiago Y Oliveira, Deena A Oren, Victor Ramos, Lilian Nogueira, Eleftherios Michailidis, Davide F Robbiani, Anna Gazumyan, Charles M Rice, Theodora Hatziioannou, Paul D Bieniasz, Marina Caskey, Michel C Nussenzweig bioRxiv 2020.09.09.288555; doi: https://doi.org/10.1101/2020.09.09.288555
- Peer reviewed and published scientific report.
Wang, Zijun, Julio C. C. Lorenzi, Frauke Muecksch, Shlomo Finkin, Charlotte Viant, Christian Gaebler, Melissa Cipolla, et al. 2021. “Enhanced SARS-CoV-2 Neutralization by Dimeric IgA.” Science Translational Medicine 13 (577). https://doi.org/10.1126/scitranslmed.abf1555. https://www.science.org/doi/10.1126/scitranslmed.abf1555.