Some people are at a higher risk of having severe coronavirus disease (COVID-19), the illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). These include older adults and those with underlying medical conditions, such as obesity, lung disease, and cardiovascular disease.
A team of researchers at the Center for Infectious Disease and Vaccine Research, La Jolla Institute for Immunology (LJI) explains why some people are more susceptible to the effects of the virus, developing the severe disease than others. In some people who contract the virus they develop only mild to moderate symptoms, while some have no symptoms at all. In other groups of people, they develop severe disease and are more likely to die from the infection.
In the new study, published in the journal Cell, the team has found that the uncoordinated responses produced by the immune system, especially in people who are more than 65 years old, maybe the reason why older adults are more at risk.
.jpg)
Activation of T-cell leukocytes. T-cell encounters its cognate antigen on the surface of an infected cell. T cells direct and regulate immune responses and attack infected or cancerous cells. Image Credit: Designua / Shutterstock
Weak or uncoordinated response
The power of the immune system to work properly and in a coordinated manner is critical in fighting the SARS-CoV-2 infection early in the acute phase of the infection. This way, COVID-19 severity will be reduced, preventing the development of severe disease and mortality.
In the study, the researchers noted that the T cells or T lymphocytes, which are one of the significant components of the adaptive immune system, play a more prominent role in the response against the coronavirus than antibodies. T cells work by killing infected host cells and activating other immune cells, producing cytokines, and controlling the immune response.
When there is a weak or uncoordinated immune response, it may lead to a poor disease outcome. The study findings reveal that potential vaccines against SARS-CoV-2 should elicit a broad immune response, including antibodies, killer T cells, and helper T cells, to make sure they can provide efficient and protective immunity.
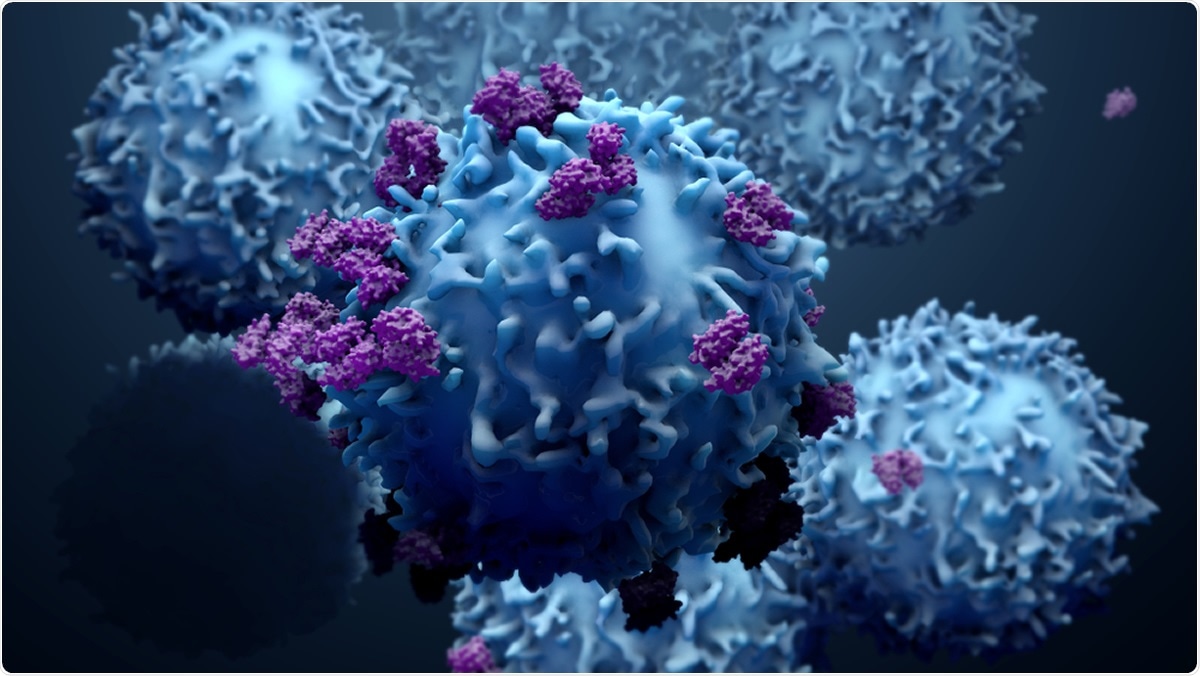
Image Credit: Design_Cells / Shutterstock
Study findings
To arrive at the study findings, the team analyzed the blood of 24 people with varying COVID-19 cases. Some had mild disease, while others were critically ill. The team compared the immune responses with 26 patients who have recovered from the disease and a control group, consisting of 65 people who have never been infected with SARS-CoV-2.
The blood samples were examined to analyze the three branches of the adaptive immune system – SARS-CoV-2 specific antibodies, helper T cells, and killer T cells. Helper T cells (Th) assist B cells in producing protective antibodies, while killer T cells (CTL) seek out virus-infected cells and kill them.
The team has found that patients who recovered from the disease had measurable antibody, helper, and killer T cells responses. The adaptive immune response varied broadly with some people lacking neutralizing antibodies, while others lack killer or helper T cells, or any combination of them.
Why are some people more vulnerable?
Overall, patients with mild disease who produced a more vast and well-coordinated adaptive response had a better prognosis. When the team analyzed the findings by age, those who are over 65 years old have more deficient T cell responses and an uncoordinated immune response, making their illness more severe or fatal, compared with others.
Older adults appear to have weak adaptive immune responses since they have fewer naïve T cells. For this reason, they are more susceptive to developing severe disease, not just from the novel coronavirus, but for other viral diseases, as well.
The team also emphasized that the antigen-specific antibody and T cell data suggest that adaptive immune responses limit COVID-19 disease severity, coordinated responses by all three of the branches adaptive immunity provides better protection, and CXXL10 may be a plasma marker in acute COVID-19 of impaired T cell responses. Further, aging and scarcity of the naïve T cells may be tied as risk factors for the body's immune system to work in a coordinated manner.
"Our observations could also explain why older COVID-19 patients are much more vulnerable to the disease," Dr. Shane Crotty, a professor in LJI's Center for Infectious Disease and Vaccine Research, sad.
"With increasing age, the reservoir of T cells that can be activated against a specific virus declines and the body's immune response becomes less coordinated, which looks to be one factor making older people drastically more susceptible to severe or fatal COVID-19," Crotty added.
The researchers hope that the findings may be considered by scientists and institutions who are formulating vaccines against COVID-19. Vaccine makers should concentrate more on T cell responses to ensure that the vaccine can help protect people from all ages, including older adults.
Source:
Journal reference: