In the northern hemisphere, the flu season is just around the corner as winter fast approaches. With the expected surge in influenza illness and coronavirus disease (COVID-19) cases, health experts warn high-risk people to take precautions, including pregnant women.
The study, published in the Proceedings of the National Academy of Sciences (PNAS), shows that influenza A virus (IAV) infection during pregnancy causes severe maternal and perinatal complications, despite the lack of vertical transmission across the placenta. Even if the virus does not affect the fetus directly, it could still lead to severe complications in the mother's body.
The study provides new information on why some mothers and their unborn babies develop severe complications during a flu infection, and it could help scientists who are working to understand better how COVID-19 spreads from the lungs to the other parts of the body.
Spreading through circulation
The study findings, which came from experiments with animal models, highlight how the virus can travel from the lungs and into other systems, potentially causing severe illness. The team said that from the lungs, the virus travels via the blood vessels and into the circulatory system, inducing a damaging hyperactive immune response.
The team observed the effect of the virus on non-pregnant and pregnant mice. Interestingly, they found that in non-pregnant mice, the infection was self-resolving and was only contained in the lungs.
On the other hand, in pregnant mice, the virus has found its way to other parts of the body through major maternal blood vessels, including the aorta, resulting in inflammation. Healthy blood vessels dilate about 90 to 100 percent to let blood flow freely, while flu-infected blood vessels dilate or function at only 20 to 30 percent of capacity.
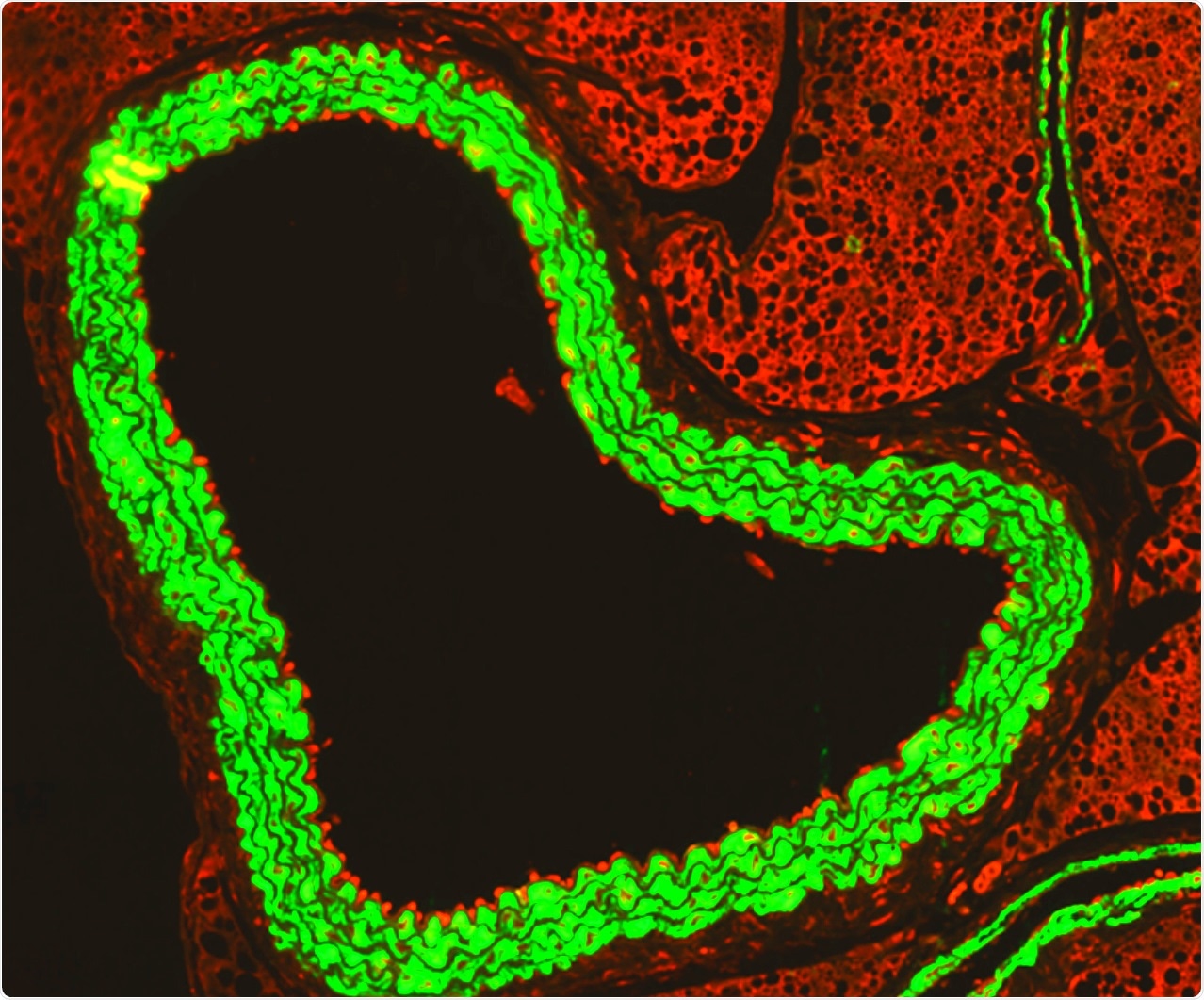
An immunofluorescence microscopy image shows how activated immune cells (red) ‘stick’ to the inside of the aorta (green) during flu infection in pregnancy.
As a result, the spread has triggered a peripheral vascular storm, with increasing proinflammatory and antiviral mediators and the influx of white blood cells. Aside from a vascular storm, blood circulation has been affected.
The study suggests that the vascular system is the center of potentially devastating complications caused by influenza during pregnancy.
"We've known for a long time that flu can cause serious maternal and fetal complications, but how this happens has not been clearly understood," Dr. Stella Liong, a Vice-Chancellor's Postdoctoral Fellow at RMIT, said.
"Conventional thinking has blamed the suppressed immune system that occurs in pregnancy but what we see is the opposite effect - flu infection leads to a drastically heightened immune response. The inflammation we found in the circulatory system is so overwhelming. It's like a vascular storm wreaking havoc throughout the body," she added.
She added that further studies are needed to validate the new mechanism, which can help develop new therapies for flu, particularly for pregnant women.
"The discovery of an influenza-induced 'vascular storm' is one of the most significant developments in inflammatory, infectious diseases over the last 30 years and has significant implications for other viral infections, including COVID-19," Professor John O'Leary, Trinity College Dublin, said.
Pregnancy complications
During pregnancy, the placenta secretes proteins and fetal DNA into the mother's blood, leading to underlying inflammation. In the new study, the team said that flu infection might push the inflammation over the edge, causing a full-blown systemic inflammatory event.
The influx and elevated levels of adhesion molecules induced by the vascular storm caused a profound vascular dysfunction, which may lead to placental growth retardation and intrauterine growth restriction. Other complications may include evidence of placental and fetal brain hypoxia or the lack of oxygen in the fetal brain, and the increased circulating free fetal DNA and soluble Fms Related Receptor Tyrosine Kinase 1(FLT1), which has been linked to pre-eclampsia, a dangerous pregnancy complication characterized by elevated blood pressure and may cause maternal seizures.
"Therefore, IAV infection during pregnancy drives a significant systemic vascular alteration in pregnant dams, which likely suppresses critical blood flow to the placenta and fetus. This study in mice provides a fundamental mechanistic insight and a paradigm into how an immune response to a respiratory virus, such as IAV, is likely to specifically drive maternal and fetal pathologies during pregnancy," the researchers concluded in the study.
The researchers believe that the study could pave the way for developing drugs that target vascular inflammation, which can help pregnant women who have flu infection.