A recent study conducted in the Atlanta area reveals that coronavirus disease 2019 (COVID-19) related sexual distancing together with clinical service interruption for sexually transmitted diseases can potentially impact the future incidence of the human immunodeficiency virus (HIV) and other sexually transmitted infections (STIs). The study is currently available on the medRxiv* preprint server.
Since its emergence, the COVID-19 pandemic has put severe burdens on the healthcare system and economy of many countries worldwide. In addition, control measures that have been applied to contain the pandemic, such as social distancing, has indirectly impacted the spread of HIV and other STIs by reducing sexual activities. Another crucial impact of the pandemic is an interruption in clinical services for HIV/STIs.
In the United States, sexual activity between male partners is the primary cause of HIV/STI transmission. However, because of the COVID-19 related restrictions, a reduction in the numbers of partners, as well as frequency of sexual activity, has been observed among men who have sex with men (MSM). Simultaneously, HIV/STI related clinical services, such as diagnostic screening, utilization of preexposure prophylaxis, and continuation of therapies, have been reduced among MSM in the US regions with high HIV/STI prevalence, such as Atlanta.
In the current study, the scientists from Emory University, the University of North Carolina, and Harvard Medical School tried to determine the combined impact of sexual distancing-related reduction in transmission and service interruption-related induction in transmission on the overall incidence of HIV/STIs in the long run.
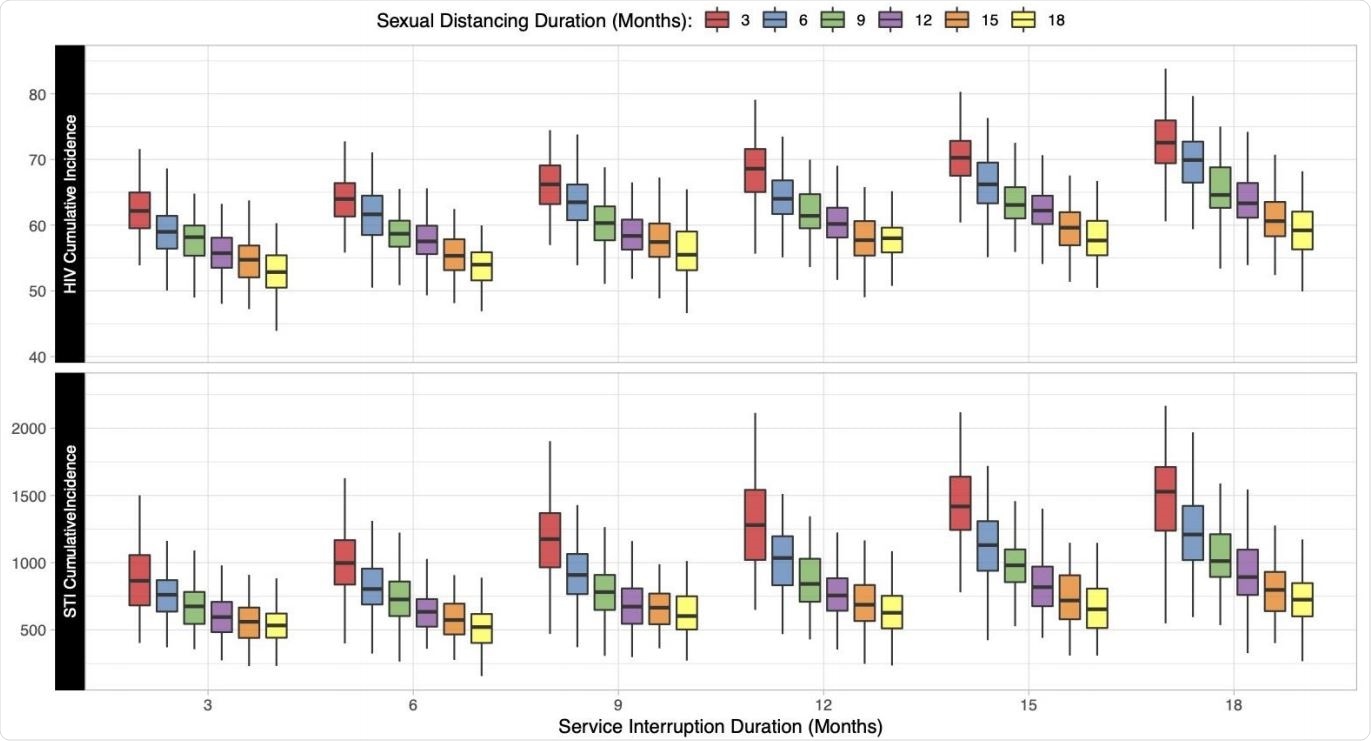
Relationship between the duration of sexual distancing and service interruption on cumulative (5-year) incidence of HIV and STIs per 1000 susceptible MSM. Individual boxes display the distribution of 500 simulations across each scenario.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Current study design
In the study, a network-based model of co-circulating HIV, gonorrhea, and chlamydia was adopted for black, Hispanic, and white MSM population (age range: 15 – 65 years) who live in Atlanta. The scientists evaluated the impact of COVID-19 related alteration in sexual partnership behaviors (main, casual, and onetime relationships) on the overall incidence of HIV/STIs. Moreover, they investigated how COVID-19 related service interruption (HIV screening, HIV preexposure prophylaxis, HIV treatment, and STI treatment) may impact the HIV/STI trajectories over the next 5 years.
Important observations
The scientists observed that reduction in clinical service and partnership network by 50% for 18 months mostly counterbalanced the effects of each other for HIV; however, the same situation was found to have a positive impact on STI incidence.
A reduction in clinical service for a prolonged period of time was found to be associated high higher incidence of HIV and STIs; whereas, a reduction in HIV/STI incidence was observed with long-term sexual distancing. Of various clinical services, interruption in antiretroviral therapy-related services for HIV patients was found to have the maximum impact on the estimated increase in HIV cases. Based on the study model situation of 3 months of sexual distancing together with 18 months of clinical service reduction, the scientists estimated that there would be an additional 900 and 57,000 cases of HIV and STI, respectively, among the MSM population over the next 5 years in Atlanta. This indicates that although practicing sexual distancing has a counterbalancing effect on service interruption, the timing of these changes is important in determining the incidence rate for HIV/STIs. A short-term change in sexual behavior, together with long-term service interruption, can actually increase the incidence rate.
Overall, the study projections indicate that a reduction in the number of sexual partners, together with long-term sexual distancing, has a strong effect in reducing the incidence of both HIV and other STIs. In contrast, long-term interruption in clinical services in the absence of sexual distancing can significantly increase the incidence of these infections.
However, these findings are restricted to the MSM population that has a higher baseline incidence of HIV and other STIs and lower baseline access to HIV/STI related clinical services. Thus, additional studies are required to extrapolate the data for other populations.
Study significance
The study findings signify the indirect impact of the COVID-19 pandemic on the prevention and management of other infectious diseases. This demands improved government policies to ensure uninterrupted clinical services. A step should also be taken to create awareness about protective sexual behaviors during the COVID-19 pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources