The COVID-19 pandemic has triggered intensive research into the factors that worsen the clinical phenotype, including host, environmental and genetic factors. A recent study published on the preprint server medRxiv* in October 2020 reports the potential contribution of vitamin D deficiency to an increased risk of COVID-19 in a subset of health care workers in the UK.
Vitamin D3 deficiency (VDD) results in dysregulated immunity, shown in the form of changes in the form and function of immune cells, especially lymphocytes and monocytes, which render the host especially vulnerable to infection. It is found to be very common in patients with bacterial sepsis and increases the risk of acute respiratory distress syndrome (ARDS) in such patients.
ARDS is known to be a prequel to death in ICU patients hospitalized with COVID-19. Severe illness itself promotes vitamin D deficiency, perhaps because of disruption in the normal metabolism of this vitamin.
Vitamin D is involved in synthesizing a potent steroid hormone that participates in many and varied cellular reactions in many organs. This may explain how it is required for resisting and recovering from inflammation, infection, lung disease, heart failure, and critical illness.
For one, it may promote the generation of antimicrobial compounds in the respiratory mucosa, and has been shown to reduce viral infections of the respiratory tract. It may also attenuate the host response to SARS-CoV-2 after infection occurs. At present, the prevalence of COVID-19 is unduly high among individuals with a Black, Asian, and minority ethnic (BAME) background, even after adjusting for demographic and socioeconomic characteristics, and for the existence of chronic illnesses. However, this group also has an increased risk of VDD.
Again, the risk group for COVID-19 mortality is proportional to the distance from the equator, raising the question of whether sunlight exposure and VDD plays a role in this pattern.
VDD and COVID-19 Risk
The current study follows research indicating that shift workers in the healthcare arena, outside the UK, have a greater risk of VDD than those who work only during the daytime. Junior staff are also at higher risk than those in practice or senior physicians. The study aimed to assess the prevalence of VDD in NHS workers in the UK who isolated for symptoms similar to those of COVID-19, concerning their demographic and occupational characteristics, self-reported symptoms, and the prevalence of actual COVID-19 vs. those with normal vitamin D levels.
There were ~390 healthcare workers in the study. With a median age of 41 years, almost 75% were female, and over 70% white. More than 60% had other chronic illnesses. The level of vitamin D3 was ~56 nmol/l on average. About 16% had VDD, with a mean of 22·0 nmol/l in the vitamin D deficient group vs. ~ 59 nmol/l in the non-deficient group.
The researchers found that being from a BAME background increased the odds of VDD 9-fold, while the chances of being seropositive for COVID-19 were doubled. Using this model, about 78% of cases of VDD were predicted.
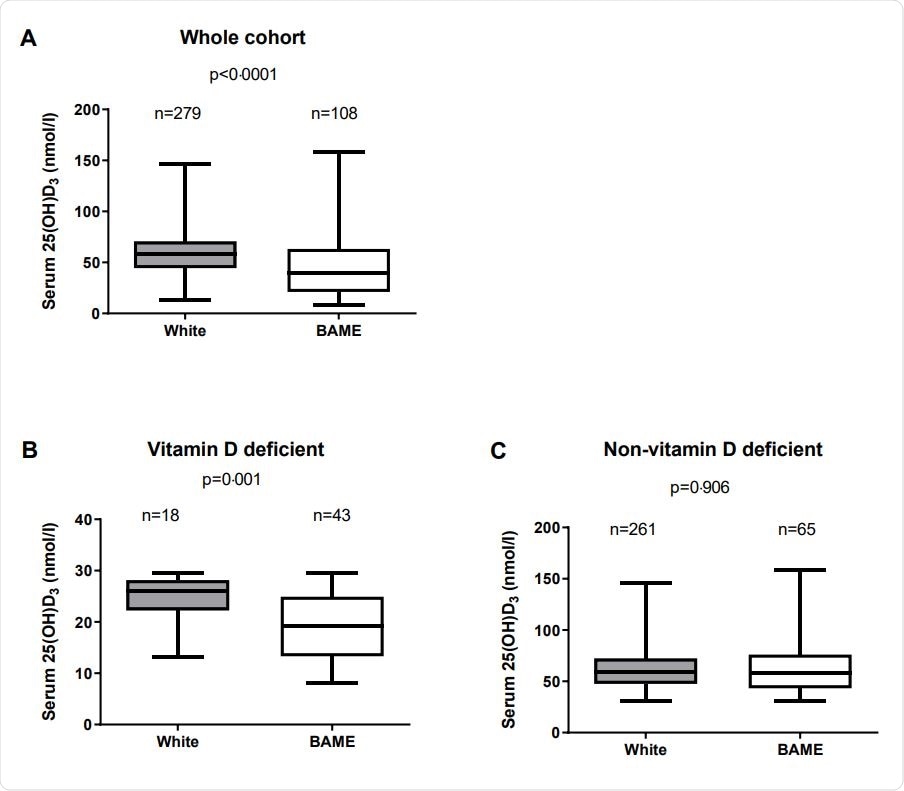
Serum D3 concentration in white and BAME staffs

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Low Symptom Correlation with VDD
Among the 386 patients who self-reported symptoms, a third had a cough, the same percentage had diarrhea, but twice that number had a fever. Almost half of them had difficulty in breathing, with the same number having a sore throat. Over 70% had body pain, almost 90% reported tiredness, and ~45% had abnormalities of taste or smell. Six patients, all with regular vitamin D3 levels, had no symptoms.
About 82% of the VDD group had symptoms like body ache vs. ~70% of the other group. Still, the symptom itself did not predict a lower vitamin D3 level compared to the whole group without this symptom, or to seropositive staff. Other symptoms, even those more characteristic of COVID-19 respiratory infection such as fever and cough, showed no significant difference.
Those with VDD were more likely to be seropositive, at 72% vs ~50%, but the serum levels were not different between seropositive and seronegative workers. This could be because the percentage of seropositives is similar in white and BAME workers with and without VDD. In the latter group, however, males with VDD were more likely to be seropositive (94%) vs. those without, at 52%.
VDD Predicts COVID-19 Seroconversion
The only significant risk indicator for COVID-19 seropositivity was VDD, which predicted over half of all cases, independent of sex, age, BMI, chronic illnesses, ethnicity, and occupation. This is the first time researchers have shown that seropositivity for COVID-19 indicates a higher risk for VDD.
This agrees with an earlier observational study showing that “testing positive for COVID-19 was inversely related to vitamin D levels.”
Implications
VDD is associated with a 45% increased risk of testing positive for COVID-19, and double the odds of requiring hospitalization for the disease. The implication could be either that the risk of COVID-19 is higher with VDD, or that COVID-19 induces VDD as in other critical illnesses. The finding that BAME individuals are more likely to have VDD agrees with earlier studies.
The researchers comment, “While BAME was not an independent risk factor for seroconversion in this cohort, vitamin D deficient BAME male may be the group most at risk from COVID-19.”
All individuals in this cohort had mild COVID-19, but nonetheless, this shows that BAME males are at a higher risk for a poor outcome if they require ICU admission with COVID-19.
The authors point out that “These data raise the question of whether vitamin D supplementation in vitamin D deficient individuals may help alleviate the impact of SARS-Cov-2 if infected.” Some findings of a recent trial seem to indicate that this is a direction worth following.
More research is needed to validate these findings in other settings and a larger cohort, with a broader spectrum of disease and diverse ethnic backgrounds.
However, given that BAME males are at higher risk of VDD and that this is a factor for COVID-19 infection, it would seem that supplementation with vitamin D, which is both cheap and readily available, as well as safe, is worth a try in order to alleviate the risk, especially in clinical trials.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Faniyi, A. A. et al. (2020). Vitamin D Status and Seroconversion For COVID-19 In UK Healthcare Workers Who Isolated For COVID-19 Like Symptoms During The 2020 Pandemic. medRxiv preprint. doi: https://doi.org/10.1101/2020.10.05.20206706. https://www.medrxiv.org/content/10.1101/2020.10.05.20206706v1
- Peer reviewed and published scientific report.
Faniyi, Aduragbemi A., Sebastian T. Lugg, Sian E. Faustini, Craig Webster, Joanne E. Duffy, Martin Hewison, Adrian Shields, Peter Nightingale, Alex G. Richter, and David R. Thickett. 2020. “Vitamin D Status and Seroconversion for COVID-19 in UK Healthcare Workers.” The European Respiratory Journal, December. https://doi.org/10.1183/13993003.04234-2020. https://erj.ersjournals.com/content/57/4/2004234.