Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pathogen, has infected over 55.1 million people around the world, and severe forms of the disease have caused more than 1.31 million deaths.
As yet, no specific and effective antiviral drugs are available to treat the severe form of the disease. Similarly, no effective and safe vaccines that could immunize against SARS-CoV-2 are available for use by the general population – and those vaccine candidates currently entering their final stages of approval may not be widely distributed for some time.
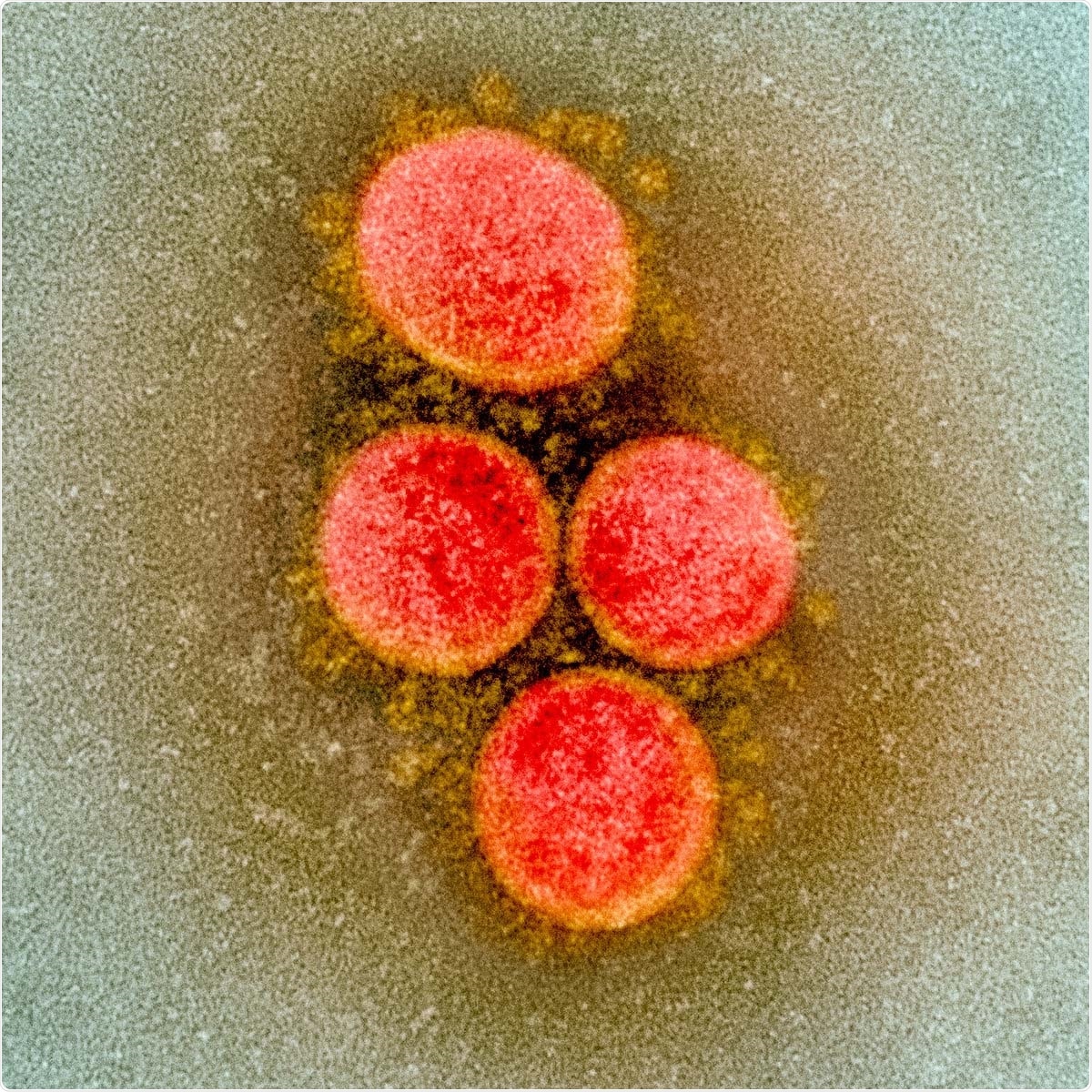
Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Image Credit: NIAID / Flickr
Researchers from the Department of Critical Care Medicine, Sichuan Provincial People's Hospital, Chengdu in China, have explored the possibility of using hydrogen therapy on severely ill COVID-19 patients. The team published their study's findings, titled "Hydrogen: A Potential New Adjuvant Therapy for COVID-19 Patients," in the latest issue of the journal Frontiers in Pharmacology.
Background
The authors explained that hydrogen possesses properties such as antioxidant, anti-inflammatory and hormone-regulating actions. It can also help resist immune-led apoptosis (or programmed cell death) among cells of the body.
SARS-CoV-2 is known to cause cytokine storms or severe inflammatory action in some individuals. This form of cytokine storms is often seen in severe COVID-19 cases and can often result in fatalities. Cytokine storms are known to cause damage to the lungs. Hydrogen therapy, the researchers write, is known to cause "ropy sputum drainage," which reduces the intensity of the disease and can also help as an adjuvant therapy in severe disease.
Inflammatory markers
In severe COVID-19, the team explains, there is a marked rise in plasma levels and of inflammatory markers such as IL-2 (Inter Leukin), IL-7, IL-10, and TNF-α (Tumor necrosis factor). At present, cytokine storms where these features are seen, have no specific treatments.
Hydrogen therapy
The team writes that hydrogen is a "colorless, odorless, and tasteless gas." In 2007, a study published in Nature, showed that inhalation of two percent hydrogen could specifically eliminate the hydroxyl radical (OH) and peroxynitrite anion (ONOO−). Among rats with ischemic injury to the brains, this inhalation could help in reperfusion and correction of ischemic injury, found the researchers. The researchers of the present study note that since then, hydrogen therapy has gathered a lot of interest among researchers and critical care specialists.
The team writes that hydrogen has properties such as "anti-oxidation, anti-inflammation, anti-apoptosis, and hormone regulatory" and thus could potentially find utility in several diseases. Moreover, being small, the hydrogen molecule is capable of reaching the alveoli and thus could help in lung diseases,
Cytokine storm
In cytokine storms, there is a rise in pro-inflammatory cells and mediators called cytokines such as tumor necrosis factor-α (TNF-α), interleukins (such as IL-1β and IL-6), and interferon-γ (IFN-γ).
Once activated, these cytokines activate the NADPH oxidase in leukocytes or white blood cells. This, in turn, gives rise to reactive oxygen species (ROS), including "superoxide, hydroxyl radicals, and singlet oxygen." These are known to cause damage to several organs.
SARS-CoV-2 induces an interferon-γ-related cytokine storm that leads to severe disease. This form of cytokine storm has also been seen in avian influenza A H5N1 (caused by high viral loads) and Middle East respiratory syndrome (MERS), a betacoronavirus in the same family as SARS-CoV-2. It is usually caused due to high IL-1 β, INF-γ, IP-10, MCP-1, G-CSF, MIP-IA and TNF-α.
Hydrogen as treatment option
As treatment options for severe COVID-19, several drugs are being tried, including tocilizumab and dexamethasone. Studies have also tried anti-IL6-receptor therapy among these patients. Some researchers have also found that hydrogen can suppress the inward infiltration of the WBCs such as neutrophils and macrophages in lung tissue and also block the action of NF-κB and MPO in lung tissue. It reduces the inflammatory factors and also reduces the cytokine secretion in lung tissue, including TNF-α, IL-1, IL-6, and HMGB1. Hydrogen also removes the ROS, including hydroxyl and peroxynitrate anions and restores normal metabolism of the redox reactions and other ROS.
Thus studies have shown, wrote the researchers, "hydrogen treatment can reduce the levels of TNF-α, IL-1, IL-1 β, IL-6, IL-8, HMGB1, CCL2, and Egr-1 in lung tissue in an animal model". In 45 minutes, hydrogen inhalation can reduce the airway inflammation seen among asthma and COPD patients. The team added, "hydrogen can inhibit the Rho/ROCK pathway, increase the expression of ZO-1, and protect lung tissue cells by improving cell-to-cell permeability, and reducing lung injury."
They thus speculate that hydrogen could play a role in therapy for severe COVID-19 patients with lung injury.
Hydrogen and its effects on oxidative stress
Superoxide dismutase (SOD) is an enzyme that works by protecting the body against antioxidant damage, explain the researchers. Hydrogen therapy has been found to reduce the amounts of malondialdehyde in lung tissues and thus increase the action of SOD.
The researchers state that critically ill COVID-19 patients often develop multiple organ failure and that hydrogen, due to its properties of antioxidation and anti-apoptosis, could help protect several organs in the body, including the heart, the kidneys and the nervous system.
Hydrogen reduces the viscous secretions seen in COVID-19
In lung injuries caused by inflammation, viscous secretions fill up the alveoli and clog up the terminal bronchi. Oxygen use given using nasal high-flow oxygen inhalation and non-invasive ventilator-assisted ventilation can help the patients. The researchers added that this positive pressure ventilation mode could also lead to the accumulation of viscous bronchial secretions and ultimately worsen the hypoxia or lack of oxygen at the terminal bronchi.
Hydrogen-enriched water, when used in mucus secretion in smog-induced COPD models of rats, has shown that there is reduced secretion and relief of hypoxia. The team writes, "early hydrogen inhalation may promote sputum dilution, improve small airway resistance, and relieve dyspnea."
How safe is hydrogen therapy?
Some of the safety concerns include the fact that it is flammable and explosive, but less than 4 percent together with oxygen at room temperature is not combustible. No serious side effects are seen with hydrogen use. Some complain of heartburn, constipation and headache.
The authors believe that hydrogen therapy could be used among severe COVID-19 patients with success. They write, "In the future, more large-scale randomized controlled trials are needed to verify the efficacy and safety of this treatment clinically."