Researchers in the UK have developed a prognostic tool that accurately predicts whether patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent causes coronavirus disease 2019 (COVID-19) – will require admission to the intensive care unit (ICU), die, or survive without escalation to ICU.
The researchers say the tool discriminated well between patients who would and would not require ICU admission (or die) and was better and predicting this need than current prognostic tools.
The risk scores currently used do not generally account for the dynamic changes in severity of disease on a daily basis during the hospital admission period, say the researchers.
“We have shown that incorporating daily measurements of clinical observations and blood tests improves the accuracy of both the prediction of prognosis and of resource demand in secondary care patients with SARS-CoV-2,” they write.
If validated in other populations, the findings suggest that such a tool could provide a warning that an escalation of care and certain ICU resources are going to be needed.
A pre-print version of the paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The challenges faced by health services
Throughout 2020, the COVID-19 pandemic has placed unprecedented strain on health services, bringing some systems to a state of near collapse.
The need to redirect resources has probably increased the risk of mortality due to other illnesses, says Card and the team. As the pandemic undergoes further waves, limited resources will again need to be focused on the severely ill while trying to maintain the care of patients with other health problems.
During the first wave of the pandemic, a number of prognostic and prioritization scores were developed.
“Ideal scoring systems would allow safe and early discharge of those that would not be likely to require ongoing hospital care, while at the same time enabling prompt escalation of care for those with deteriorating disease,” say the researchers.
The scores currently used are generally based on clinical and laboratory parameters measured at a single time point (usually hospital admission), but clinical decisions regarding escalation of care must be made throughout the disease course.
Some scores are designed for more dynamic use through the disease course, but they are not disease-specific, says Elliott and colleagues.
“A simple score which is intended to be both dynamic and optimized for SARS-CoV-2 might, however, be expected to perform better and with levels of disease rising again such a scoring system would be of great value,” they write.
What did the researchers do?
The team conducted a retrospective, observational study of all patients with confirmed SARS-CoV-2 infection who were admitted to Nottingham University Hospitals (NUH) NHS Trust between 1st February and 30th November, this year (2020).
Patients (n=2,964) were divided into a first wave group (those admitted up to 30th June; n=1,374) and a second wave validation group (those admitted thereafter; n=1,590).
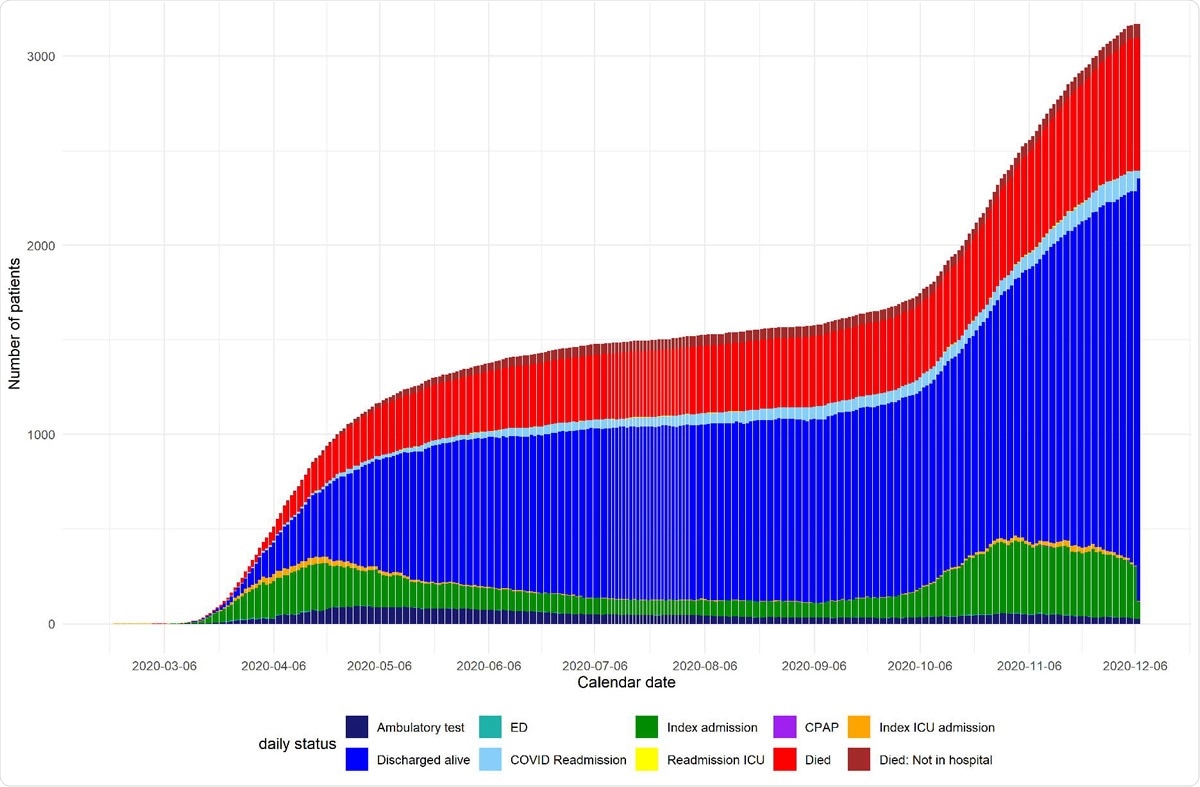
Daily status of patients from day of suspected COVID diagnosis
The NUH electronic records incorporate comprehensive sociodemographic, clinical and laboratory variables, including all measurements recorded throughout the admission period. Complete information was also available for escalation of care, death, or for 30 days follow-up after hospital discharge.
By linking this information to baseline data at presentation, the researchers were able to retrospectively analyze the performance of scores across the whole of the admission period.
“We have therefore set out to develop a truly dynamic and SARS-CoV-2 specific score,” they write.
The model precisely predicted the need for ICU
Among the first wave group, 593 patients were eligible for ICU escalation, and among the validation group, 958 were eligible for ICU admission.
The model was able to predict the daily need for ICU admission, death or survival without escalation of care with good precision through the admission period. Furthermore, the tool predicted this daily prognosis better than previously established scores.
In the validation group, the score exhibited excellent discrimination but had to be recalibrated because it overestimated escalation and death.
“This is likely to reflect the change in demographics and clinical practice between the first and second UK wave, given changes in escalation practice and introduction of the use of steroids in patient treatment,” explains the team.
What did the researchers conclude?
The researchers say the study has shown that incorporating daily measurements of clinical observations and blood tests improves the accuracy of predicting prognosis and resource demand in secondary care patients with SARS-CoV-2.
“Clinical application of such a dynamic score could be used to prompt clinical review to ensure the timely escalation of care, and to predict the need to increase or repurpose critical care capacity at an operational level in hospitals,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Card T, et al. Predicting the need for escalation of care or death from repeated daily clinical observations and laboratory results in patients with SARS-CoV-2 during 2020: a retrospective population-based cohort study from the United Kingdom. medRxiv, 2020. doi: https://doi.org/10.1101/2020.12.14.20248181, https://www.medrxiv.org/content/10.1101/2020.12.14.20248181v1
- Peer reviewed and published scientific report.
Crooks, Colin J, Joe West, Andrew Fogarty, Joanne R Morling, Matthew J Grainge, Sherif Gonem, Mark Simmonds, et al. 2022. “Predicting Need for Escalation of Care or Death from Repeated Daily Clinical Observations and Laboratory Results in Patients with Severe Acute Respiratory Syndrome Coronavirus 2.” American Journal of Epidemiology 191 (11): 1944–53. https://doi.org/10.1093/aje/kwac126. https://academic.oup.com/aje/article/191/11/1944/6648775.