Amid the coronavirus disease 2019 (COVID-19) pandemic, healthcare workers (HCW) have been overworked and faced with the risk of being infected with severe acute respiratory syndrome coronavirus (SARS-CoV-2), the causative pathogen of COVID-19.
A new study by US-based researchers – at the Northwest Mental Illness Research, Education and Clinical Center and Columbia University – has found that healthcare workers have experienced significant psychiatric distress during the pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The coronavirus pandemic
The coronavirus pandemic first emerged in Wuhan City, China, in December 2019. Since then, it has spread to 191 countries and territories, infecting over 76.79 million and killing more than 1.69 million people.
Due to the scale and speed of the virus's spread, many countries' healthcare systems were overwhelmed, and hospitals faced a shortage of intensive care unit (ICU) beds, personal protective equipment (PPE), and personnel.
The impact of the prolonged physical and emotional stress on HCW and first responders (FR) working during the pandemic has attracted significant attention in the media. Previous studies have also tackled the physical and emotional stressors among these workers, linked with significant personal distress and decreased professional longevity.
Previous studies have tied the pandemic to higher psychiatric symptoms among healthcare workers, including depression, insomnia, anxiety, and post-traumatic stress disorder (PTSD).
A study in New York found increased use of medical leave, leading to decreased workforce availability among healthcare workers.
Significant psychiatric distress
The study, which appeared on the preprint medRxiv* server, aimed to determine the relationship between COVID-19 stressor frequency and psychiatric rating scale scores among HCW/FR. The team also wanted to determine if the psychiatric rating scale scores affect the perceived work function and work longevity.
To arrive at the study findings, the team assessed the rate of depression, insomnia, anxiety, and PTSD symptoms in both traditionally defined HCW, as well as in FR, such as police officers, firefighters, and EMTs working during the pandemic.
The study involved 118 HCWs and FR caring for COVID-19 patients in the United States. The team used the PTSD checklist (PCL5), the Patient Health Questionnaire (PHQ9) for depression, the Insomnia Severity Index (ISI), and the General Anxiety Disorder 7 (GAD7).
The team has found that 31% of the 104 participants who completed the COVID-19 occupational exposure assessment had been ill with known or likely COVID-19. Another 19% reported a close family member who had been ill with known or likely COVID-19, and 12% reported the death of a family member due to COVID-19. About 30% also said that they had underlying health conditions that placed them at an increased risk of COVID-19.
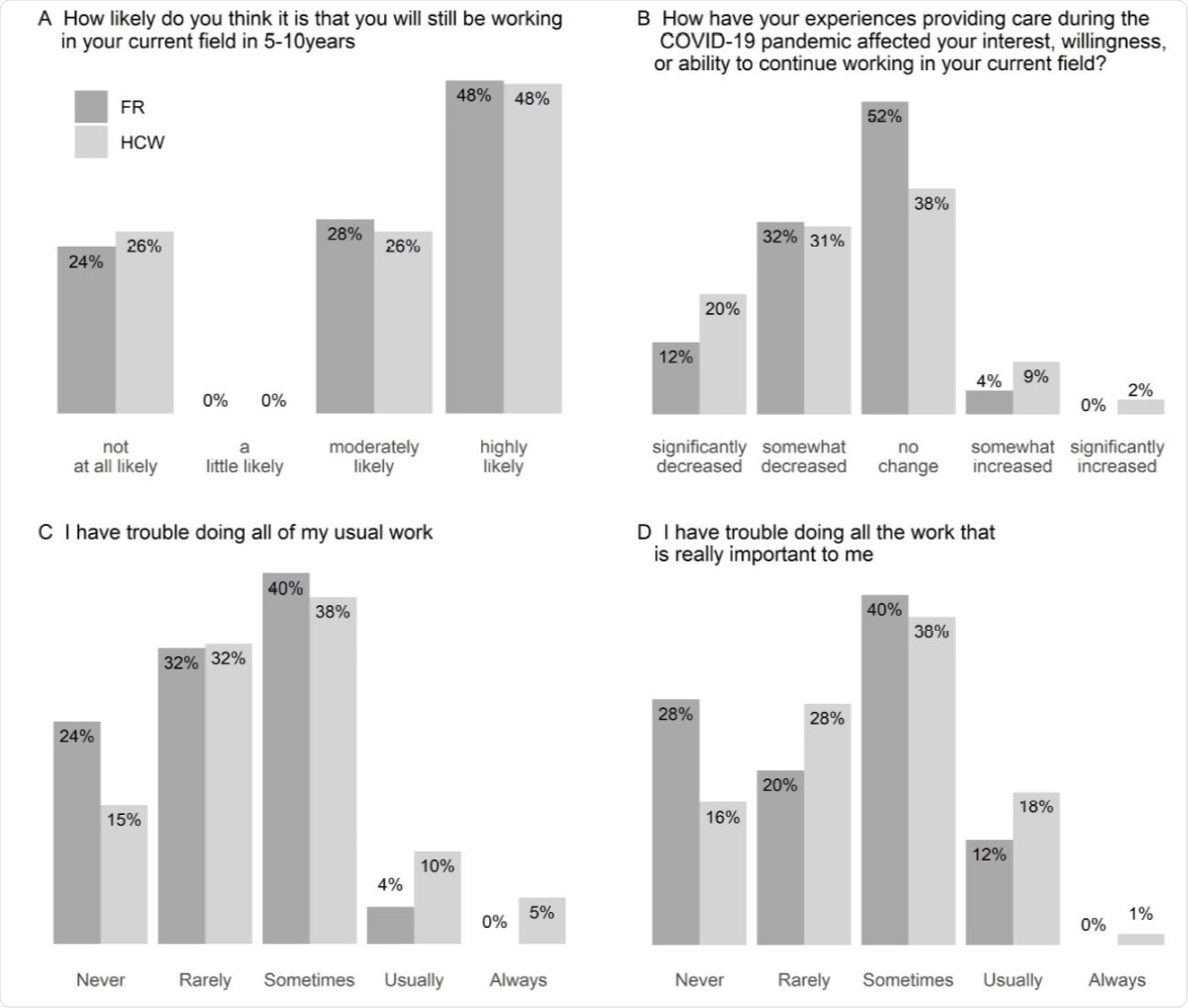
Distributions of responses to self-reported in field retention and functioning. Responses to questions about participants’ expectations regarding continuing in their current field (A,B) and current function (C,D) for health care workers (HCW, n=80) and first responders (FR, n=25).
The team revealed that 26% of the participants had a total PCL5 score of 31 or higher, indicating PTSD symptoms. These are symptoms that are usually experienced after traumatic stress. In terms of depressive symptoms, 60% of the participants had a total PHQ9 score that is above the standard threshold for mild depression, and 28% had an ISI score for least moderate insomnia. Lastly, 67% had a GAD7 score for mild anxiety.
These results direct attention to recognizing potentially treatable psychiatric symptoms, particularly those of PTSD, in HCW and FR experiencing COVID-19 related stressors," the researchers concluded.
The study findings showed that the HCW/FR's experiences during the pandemic had impacted their interest, willingness, or ability to continue working in their current field.
A substantial proportion of both groups reported their likelihood of staying in their current field had been somewhat or significantly decreased by their experiences working during the Covid-19 pandemic, and that they at least sometimes have trouble completing all of their usual or important work," the researchers added.
The researchers suggest mitigating COVID-19-related stressors among HCWs and FRs when possible, such as by providing adequate PPE and other measures. These can help improve their mental health, work function, and retention in the healthcare workforce.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Hendrickson, R., Slevin, R., Chang, B., Sano, C. E., McCall, C., and Raskind, M. (2020). The impact of working during the Covid-19 pandemic on health care workers and first responders: mental health, function, and professional retention. medRxiv. doi: https://doi.org/10.1101/2020.12.16.20248325,https://www.medrxiv.org/content/10.1101/2020.12.16.20248325v1
- Peer reviewed and published scientific report.
Hendrickson, Rebecca C., Roisín A. Slevin, Katherine D. Hoerster, Bernard P. Chang, Ellen Sano, Catherine A. McCall, Gillian R. Monty, Ronald G. Thomas, and Murray A. Raskind. 2021. “The Impact of the COVID-19 Pandemic on Mental Health, Occupational Functioning, and Professional Retention among Health Care Workers and First Responders.” Journal of General Internal Medicine, December. https://doi.org/10.1007/s11606-021-07252-z. https://link.springer.com/article/10.1007/s11606-021-07252-z.