The coronavirus disease 2019 (COVID-19) pandemic spread all over the world, reaching 191 countries and territories. Over 76.92 million cases have been reported and 1.69 million have lost their lives.
Caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pathogen, the disease can cause severe illness in older adults and those with underlying health conditions. With the sudden surge of COVID-19 cases as restrictions and lockdowns were eased or lifted towards the end of summer, healthcare systems were overwhelmed.
A new study by researchers at the Harvard T.H. Chan School of Public Health and Brown University shows that about half of US hospitals have reported reaching critical capacity since September, illustrating the scale of the coronavirus pandemic’s ‘second wave’ and the burden of pressure it has placed on the nation’s healthcare. The team’s findings have been released on the preprint medRxiv* server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The second wave of COVID-19 pandemic
As SARS-CoV-2 continues to infect more than 200,000 Americans each day, the clinical impact of all of those infections is starting to overwhelm acute care hospitals.
To date, there are more than 17.84 million confirmed cases and over 317,000 deaths in the US related to COVID-19.
Acute care hospitals are crucial in delivering care for everyone, particularly COVID-19 patients who need urgent care.
To arrive at the study findings, the researchers used newly released hospital-level intensive care unit (ICU) capacity data. The team sought to answer three pressing policy questions.
First, they wanted to know the trend in ICU capacity over the current wave or phase of the pandemic. Second, they investigated the community-level features tied to hospitals with critical ICU capacity gaps. Lastly, they looked at the structural and staffing features of hospitals with critical ICU capacity gaps.
The team assessed US acute care hospitals' data reporting to the US Department of Health and Human Services (HHS) between September 4 and December 3, 2020. They compared the data from this group to all US acute care hospitals.
Overall, 1,791 hospitals had unsuppressed ICU capacity data, with 45% reaching critical ICU capacity for at least two weeks during the study period. Hospitals located in the South, Midwest, and West were more likely to reach critical capacity than those in the Northeast.
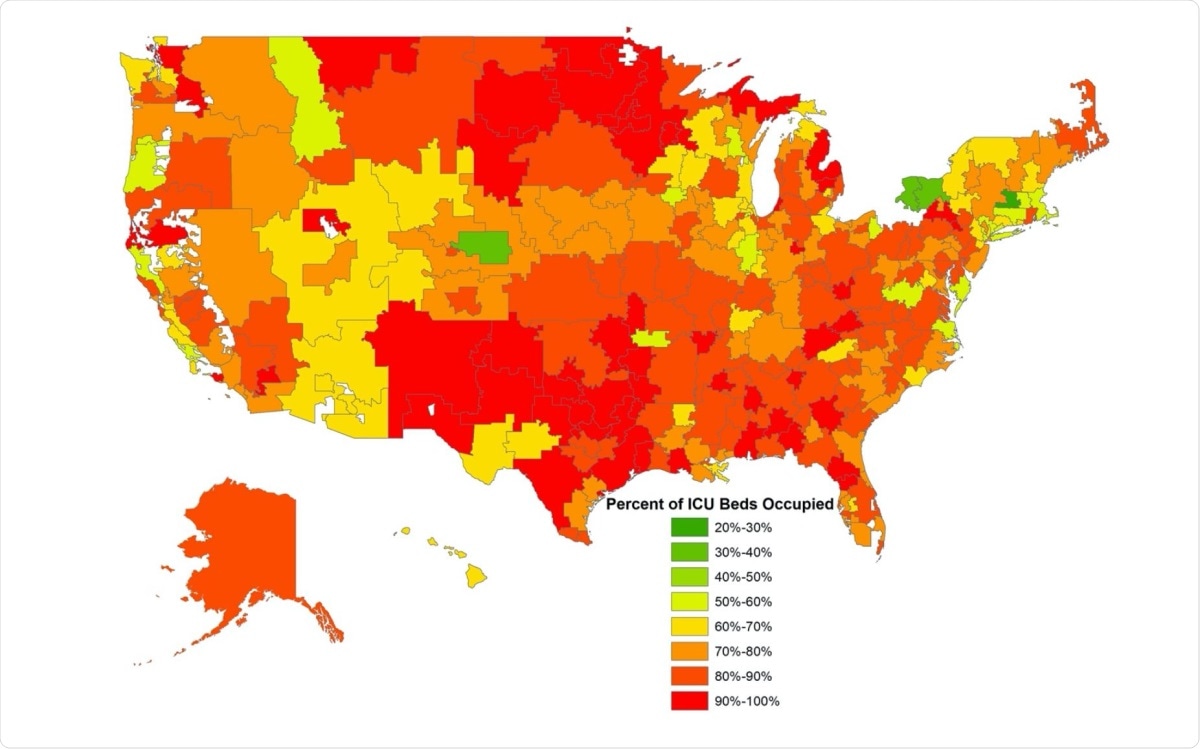
HRR-Level Geographic Variation in ICU Occupancy for the Week of November 27.
For-profit hospitals, hospitals in rural areas, and those in areas of high uninsurance were more likely to reach critical capacity. Meanwhile, hospitals with more intensivists were less likely to reach critical capacity.
“Those that are better resourced with staff were less likely to do so while for-profit hospitals and those in poorer communities were more likely to reach capacity,” the researchers concluded in the study.
“Continued non-pharmacologic interventions are needed to mitigate the spread of the disease to ensure ICUs remain open for all patients needing critical care,” they explained.
The researchers also noted that the proportion of hospitals in the Midwest with ICUs at critical capacity, which is defined as having more than 90% of beds occupied, almost tripled from 10% in September to 28% by the end of November.
Since mid-October, much of the increase has been driven by COVID-19 cases, with ICU occupied beds by coronavirus patients doubling from 9,507 to a staggering 21,203 in just five weeks.
Taken together, these results highlight the growing crisis of overburdened ICUs across the country and point to the fact that staffing and resources are likely central factors in hospitals facing the greatest threats,” the researchers noted.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Tsai, T., Jacobson, B., and Jha, A. et al. (2020). Effect of COVID-19 on Critical ICU Capacity in US Acute Care Hospitals. medRxiv. doi: https://doi.org/10.1101/2020.12.16.20248366,https://www.medrxiv.org/content/10.1101/2020.12.16.20248366v1
- Peer reviewed and published scientific report.
Tsai, Thomas C., Benjamin H. Jacobson, E. John Orav, and Ashish K. Jha. 2022. “Association of Community-Level Social Vulnerability with US Acute Care Hospital Intensive Care Unit Capacity during COVID-19.” Healthcare 10 (1): 100611. https://doi.org/10.1016/j.hjdsi.2021.100611. https://www.sciencedirect.com/science/article/pii/S2213076421000944.