A study conducted at the University of Chicago, USA, has recently revealed that downregulation of an endothelial transcription factor, Kruppel-like factor 2, by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for acute respiratory distress syndrome (ARDS) frequently observed in coronavirus disease 2019 (COVID-19) patients. The study is currently available on the bioRxiv* preprint server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
ARDS characterized by pulmonary endothelial dysfunction is one of the major complications observed in hospitalized COVID-19 patients. Lung inflammation caused by viral infections is known to downregulate Kruppel-like factor 2, which is a transcription factor required for maintaining endothelial integrity. In experimental models of ARDS, a significantly downregulated Kruppel-like factor 2 expression has been found to associate with pulmonary endothelial dysfunction and acute lung injury. Regarding the mechanism of action, Kruppel-like factor 2 increases the transcription of Rap guanine nucleotide exchange factor 3 (RAPGEF3), leading to activation of Rac1 protein and maintenance of vascular integrity.
In the current study, the scientists have investigated whether there is any association between SARS-CoV-2 infection and Kruppel-like factor 2 expression.
Current study design
The human lung autopsy samples obtained from COVID-19 patients have been analyzed using immunofluorescence assay to check the expression of Kruppel-like factor 2. Lung tissues obtained from healthy organ donors have been used as control. In addition, the expression of Kruppel-like factor 2 has been examined in mice intranasally infected with SARS-CoV-2.
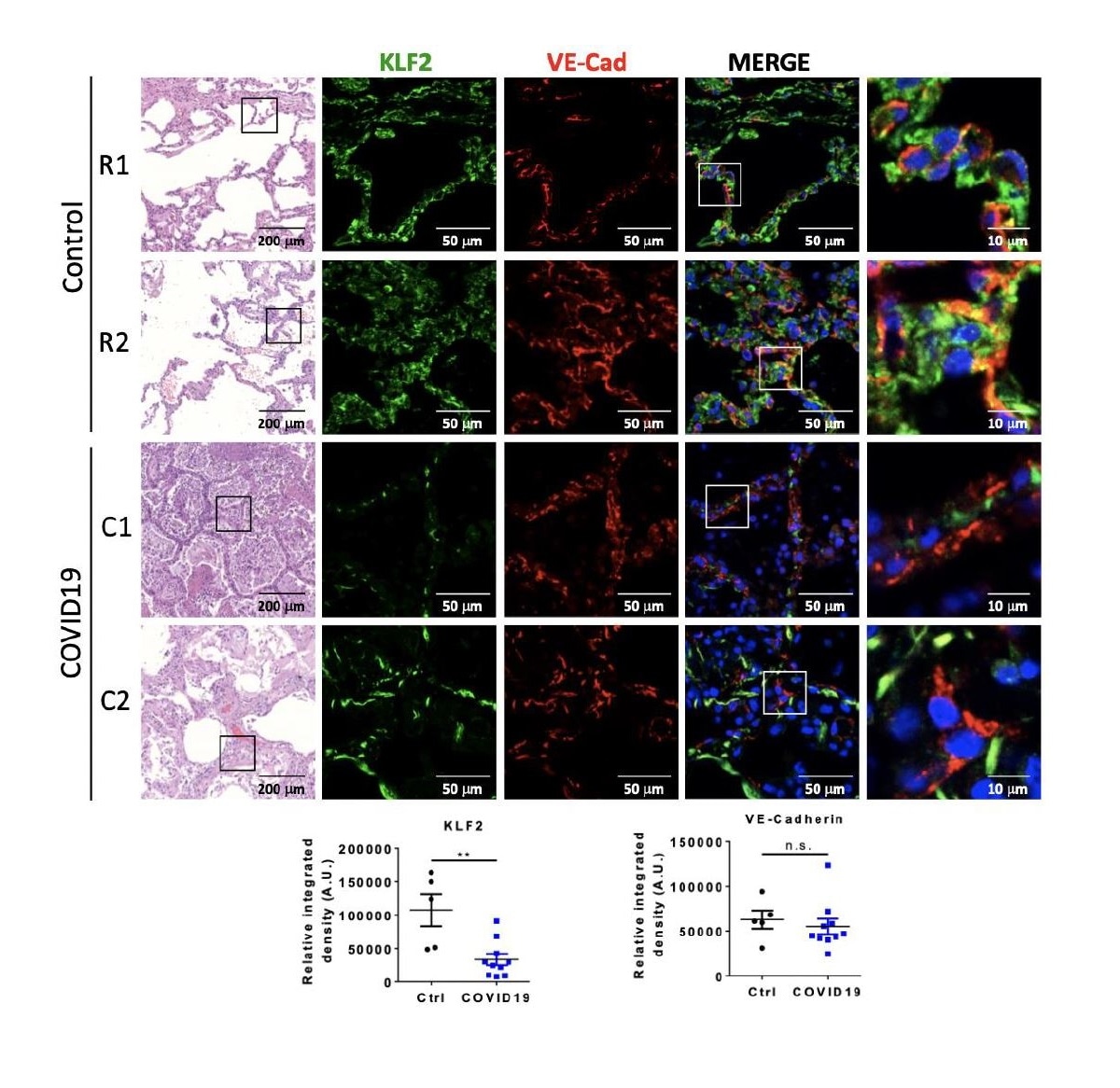
Both ROBI (R#) and COVID-19 (C#) lung autopsy samples demonstrate distorted architecture on histology. Immunofluorescence is performed for KLF2 and VE-Cad, and quantified below. In ROBI lungs, KLF2 signal (green) co-localized with VE-Cad (red), which highlights pulmonary vasculature (n = 5). In COVID-19 samples, the KLF2 signal is significantly reduced when compared to ROBI lungs (p < 0.005, n = 10). There is no significant difference in VE-Cad between ROBI and COVID-19 samples.
Important observations
The COVID-19 patients involved in the study had been diagnosed with severe acute hypoxemic respiratory failure. During the hospital stay, they had required simple or high flow nasal cannula or mechanical ventilation. These characteristics are suggestive of ARDS. According to the autopsy results, all COVID-19 patients had pathological ARDS with diffuse alveolar damage and pneumonia.
According to the current study findings, a significantly reduced expression of Kruppel-like factor 2 has been observed in the lungs of COVID-19 patients compared to that in the control lungs. The scientists have also checked the expression of vascular endothelial cadherin to define endothelial cells and have not observed any change in its expression level in the lung tissues of COVID-19 patients. These findings indicate that the reduction in Kruppel-like factor 2 expression in the lungs of COVID-19 patients is not due to the loss of endothelial cells.
In SARS-CoV-2-infected mice, the researchers observed a 40% reduction in Kruppel-like factor 2 mRNA expression in the lung tissues. Taken together, these observations indicate that SARS-CoV-2 infection can significantly reduce the expression of Kruppel-like factor 2.
Study significance
The study reveals that SARS-CoV-2-mediated reduction in Kruppel-like factor 2 is responsible for the disruption of lung vasculature, which in turn increases the risk of developing ARDS and pneumonia in severe COVID-19 patients.
There is evidence suggesting that impaired synthesis of nitric oxide is responsible for hypoxia experienced by COVID-19 patients with pneumonia. The blood flow through the lung vasculature maintains the expression of Kruppel-like factor 2, which is a transcriptional activator of nitric oxide synthase. In addition, Kruppel-like factor 2 is known to inhibit vascular thrombosis, maintaining blood fluidity. Thus, maintaining a normal Kruppel-like factor 2 expression is a prerequisite for normal pulmonary function and that SARS-CoV-2-mediated reduction in Kruppel-like factor 2 expression can significantly contribute to alveolar vascular barrier disruption, pulmonary edema formation, ischemia, and hypercoagulation.
Corticosteroids are frequently used as immunosuppressant to treat hospitalized COVID-19 patients. Alike Kruppel-like factor 2, corticosteroids suppress viral infection-induced cytokine storm in endothelium and prevent inflammation. Given this fact, the scientists suggest that corticosteroids may be used to reduce vascular inflammation and prevent vascular dysfunction in COVID-19 patients with ARDS.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources