As hospitals in many countries are filling up with coronavirus disease 2019 (COVID-19) patients, it has become a matter of great urgency to stratify the risk of critical disease and death in this group of patients.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is considered a respiratory virus but the acute illness it causes is not confined to the lungs. Rather, many terminally ill patients with COVID-19 display severe disruption of metabolic processes throughout the body, with multi-organ damage caused by underlying vascular damage and a hypercoagulable profile.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
A recent preprint research paper published on the medRxiv* server describes the alterations in lipids and other parameters that define the state of dysfunctional metabolism in acute COVID-19 illness.
Metabolic markers
The current study aims to identify at least in part a common molecular mechanism that gives rise to the protean manifestations of COVID-19. Earlier studies have shown altered liver markers, diabetes, abnormal lipid markers, and amino acid levels. Lipoprotein abnormalities are severely and consistently observed. The researchers attempted to identify whether these, and other changes, could be related explicitly to COVID-19 or whether they are common to other conditions that also affect the heart and the vascular system. They also examined the differences in metabolic profile between people who are positive for COVID-19 but have mild or no symptoms and those who are severely or critically ill.
The researchers used nuclear magnetic resonance (NMR) metabolomics to examine both the metabolic and the lipoprotein characteristics of a group of seriously ill patients with COVID-19 who were admitted to the intensive care unit (ICU) of the University Hospital of Schleswig-Holstein (Campus Lübeck), Germany, comparing these results with those from another group of healthy controls (HC), and a third group of patients without COVID-19, who were admitted in the ICU with cardiogenic shock (CS). A final group included asymptomatic individuals who tested positive for the virus.
The results of the metabolomics analysis showed clear clustering of both amino acids and lipoprotein clusters, allowing almost complete discrimination between COVID-19 patients and healthy controls. When COVID-19 patients were compared with the CS patients, the same pattern was largely repeated. With repeated testing, the gap between the clustered values for COVID-19 and other ICU patients only increased.
Energy status and lipoprotein metabolism severely disrupted
The researchers found that serum lipids were severely abnormal in COVID-19 patients alone, indicating a fundamental disturbance of the energy pathways in the body. They also found a correlation between anti-SARS-CoV-2 antibodies and metabolic markers.
The disturbed energy status is indicated by increases in glucose and formic acid levels, with a reduced lactic acid/pyruvic acid ratio, in COVID-19 patients, relative to HC. Amino acid metabolism in the liver was also perturbed, as indicated by reduced levels of glutamine, histidine and a lower Fischer’s ratio, and this was more severe in this group even compared to those with CS.
Severe dyslipidemia
Severe dyslipidemia was present in COVID-19 patients, with significant increases in very low-density lipoprotein (VLDL) and intermediate density lipoprotein (IDL), but without alteration in low-density lipoprotein levels (LDL). The high-risk marker for cardiovascular disease, ApoB100/ApoA1 (the ratio of apolipoprotein B100 to apolipoprotein A1) was also substantially higher.
In almost all lipoprotein subclasses, the triglyceride fraction was high, beginning with LDL. High-density lipoprotein (HDL) cholesterol and phospholipids were significantly reduced, with an overall reduction in HDL. This was associated with lower levels of Apo A1 and A2, and B, which are found in smaller HDL and LDL particles. Large LDL particles were increased.
When compared with CS patients, the same pattern of differentiation was observed. Increases in IDL and VLDL particles, along with lipids within VLDL, were most characteristically seen in COVID-19. Discriminatory markers that were higher in COVID-19 than in CS, included IDL triglycerides and phospholipids, VLDL-2 phospholipids and cholesterol and HDL-2 ApoA2.
Correlation with anti-SARS-CoV-2 antibodies
The above markers, namely, small LDL-6 particles and LDL-6 bound triglycerides, cholesterol, esterified cholesterol, and phospholipids, as well as small HDL 4-bound lipids, were inversely correlated with antibody levels, while glycine levels were strongly positively correlated with antibody titers.
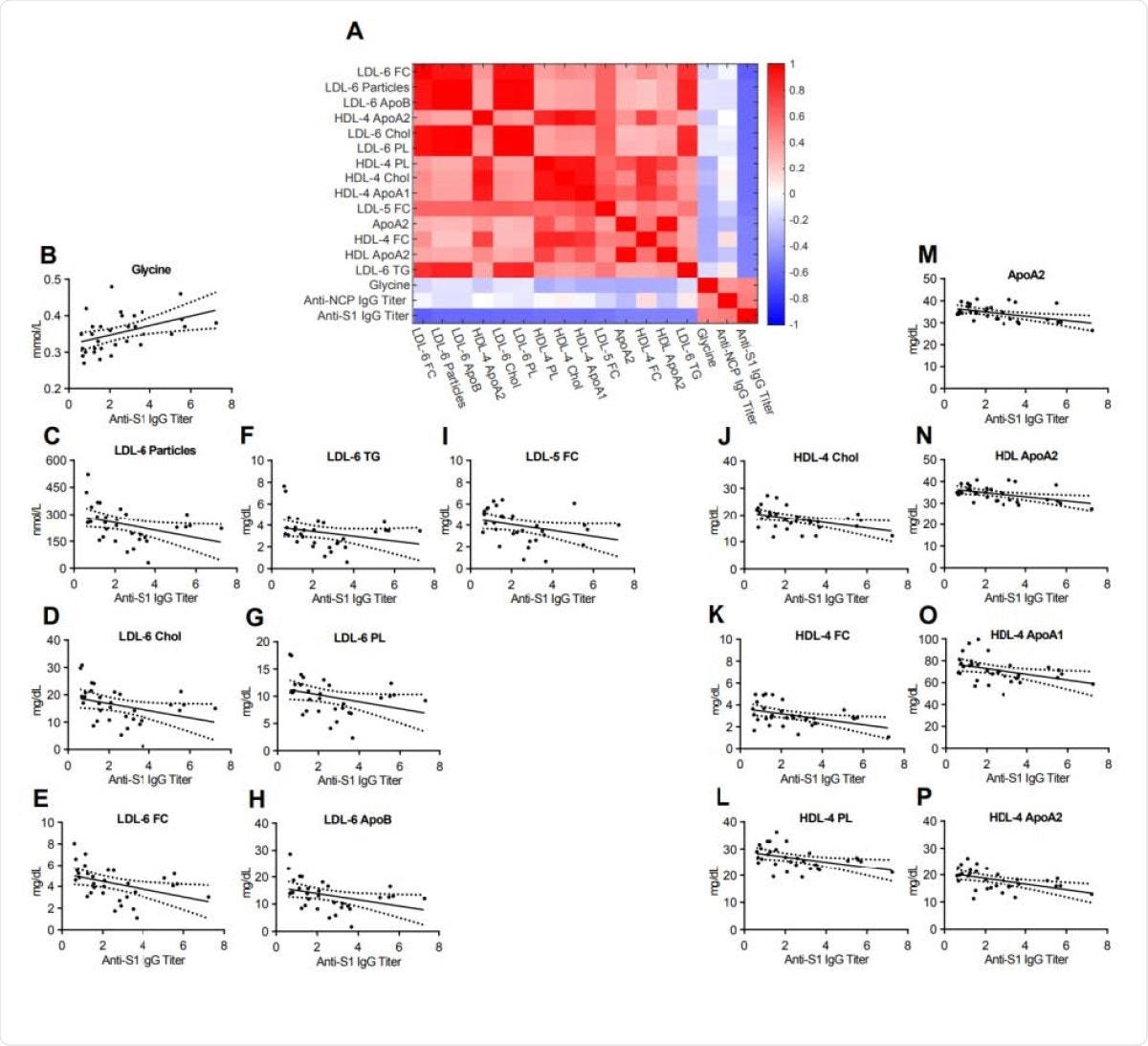
Heatmap correlating metabolite and lipoprotein levels against the Anti-S1 IgG titer for individuals who tested positive for Anti-SARS-CoV-2 antibodies (Anti-S1 IgG+). B-P. Spearman correlation plots for the most significant individual metabolites or lipoproteins against the Anti-S1 IgG titer (p- values in supplementary table).
What are the implications?
The researchers conclude that it is possible to clearly separate COVID-19 patients from either HC or CS ICU patients by their metabolic profiles. Some of these markers are not new, for instance, a lower glutamine-glutamate ratio, which is most commonly seen after anaerobic stress, in pre-cachexia in cancer, and in severe infections. This is because activated immune cells use glutamine at a rate even higher than they use sugar.
The liver in these patients, from being a large glutamine storehouse to a glutamine user, indicates a pre-cachectic state of energy. The secretion of the liver enzyme alanine-transaminase further prompts glutamine deamination to glutamate.
Phenylalanine is also increased in COVID-19, probably because the liver is the site of its metabolism to tryptophan. Glucose levels go up, histidine and methionine are reduced. While the hyperglycemia may indicate failure to use glucose for energy, and even prediabetes, the other two may indicate a failure of normal metabolism. These are not significantly altered when compared to levels in CS patients, indicating that the energy status disturbance may be due to an illness-related catabolic state.
The lipid changes seen in COVID-19 patients pose an independent risk for cardiovascular injury and disease. The high triglyceride levels are associated with atherosclerosis. Strangely, these lipids are not associated with higher concentrations of small LDL, as expected, since these patients show increases in large LDL.
Although metabolic and lipoprotein profiles fail to distinguish asymptomatic COVID-19 patients from HC, antibody titers were still related to reduced glycine and lipoprotein levels. Low glycine is inversely related to the risk of acute heart attacks in angina patients. Low glycine is being considered as a marker of metabolic stress, and as a treatment for metabolic conditions, and, intriguingly, for COVID-19.
Antibody titers against SARS-CoV-2 are also negatively associated with small LDL, indicating better metabolic health in the former case, which may be linked to higher antibody production when the infection is mild or asymptomatic. Alternatively, the changes in metabolism may indicate that the infected individual was able to fight off the infection, as shown by the higher antibody levels. This potential marker may help distinguish individuals with a greater immune response.
These results underline the severity of changes in amino acid and lipoprotein metabolism and further support the relevance of metabolic disruption by COVID-19.”
They may also indicate the utility of NMR metabolic profiles in early diagnosis and separation of the sickest COVID-19 patients from others.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Schmelter, F. et al. (2021). Metabolic markers distinguish COVID-19 from other intensive care patients and show potential to stratify for disease risk. medRxiv preprint. doi: https://doi.org/10.1101/2021.01.13.21249645, https://www.medrxiv.org/content/10.1101/2021.01.13.21249645v1
- Peer reviewed and published scientific report.
Schmelter, Franziska, Bandik Föh, Alvaro Mallagaray, Johann Rahmöller, Marc Ehlers, Selina Lehrian, Vera von Kopylow, et al. 2021. “Metabolic and Lipidomic Markers Differentiate COVID-19 from Non-Hospitalized and Other Intensive Care Patients.” Frontiers in Molecular Biosciences 8 (December). https://doi.org/10.3389/fmolb.2021.737039. https://www.frontiersin.org/articles/10.3389/fmolb.2021.737039/full.