Early on in the coronavirus disease (COVID-19) pandemic in the UK, around 6% of the national population and 13% of the London population were believed to have been infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Most of the research and media response to the pandemic focused on short-term impacts and deaths, directly and indirectly, related to COVID-19. However, more attention needs to be diverted towards the long-term effects of the disease in order to improve healthcare capacity and delivery.
Many academic and clinical works have focused on respiratory manifestations of SARS-CoV-2 infection, despite increasing evidence for multi-organ effects and indirect effects on other organs and comorbidities, such as cancers and cardiovascular diseases, due to decreased healthcare access. The epidemiology of the so-called post-COVID syndrome (PCS) is currently not clearly defined. Existing evidence shows huge variations in estimates of PCS prevalence and incidence due to variations in study populations, sample sizes, recruitment methods, and follow-up periods.
A retrospective study to determine organ impairment rates post recovery from COVID-19
In a recent medRxiv* preprint paper, researchers from the UK discussed how they determined organ impairment rates post recovery from COVID-19-related hospitalization and compared the results with that in a control group. They also analyzed how the rate ratio (RR) changes across sex, age, and ethnicity.
The observational, retrospective, matched cohort study was performed in NHS hospitals in England. The study participants included 47,780 individuals with a mean age of 65 who were hospitalized with COVID-19 and discharged by 31 August 2020. About 55% of the study cohort were male, and the cohort was matched to controls on demographic as well as clinical characteristics. The key outcomes measured were rates of all-cause mortality, hospital readmission, and diagnoses of cardiovascular, respiratory, metabolic, liver, and kidney diseases until 30 September 2020.
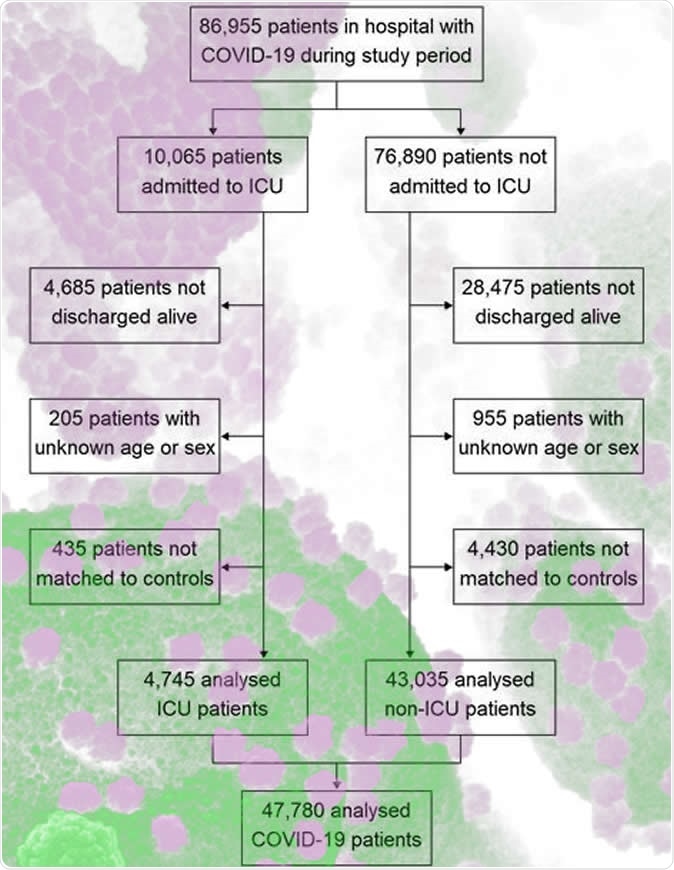
Study population flow diagram

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Individuals with PCS had higher rates of respiratory, cardiovascular, and diabetes-related events
The mean follow-up time for COVID-19 cases was 140 days, and that for controls was 153 days. In COVID-19 cases, 766 (95% confidence interval: 753 to 779) readmissions and 320 (312 to 328) deaths per 1,000 person-years were reported, which is 3.5 (3.4 to 3.6) and 7.7 (7.2 to 8.3) times greater, respectively, than that in controls.
Rates of respiratory, cardiovascular, and diabetes-related events were also considerably elevated in COVID-19 cases, with 770 (758 to 783), 126 (121 to 131), and 127 (122 to 132) events per 1,000 person-years, respectively.
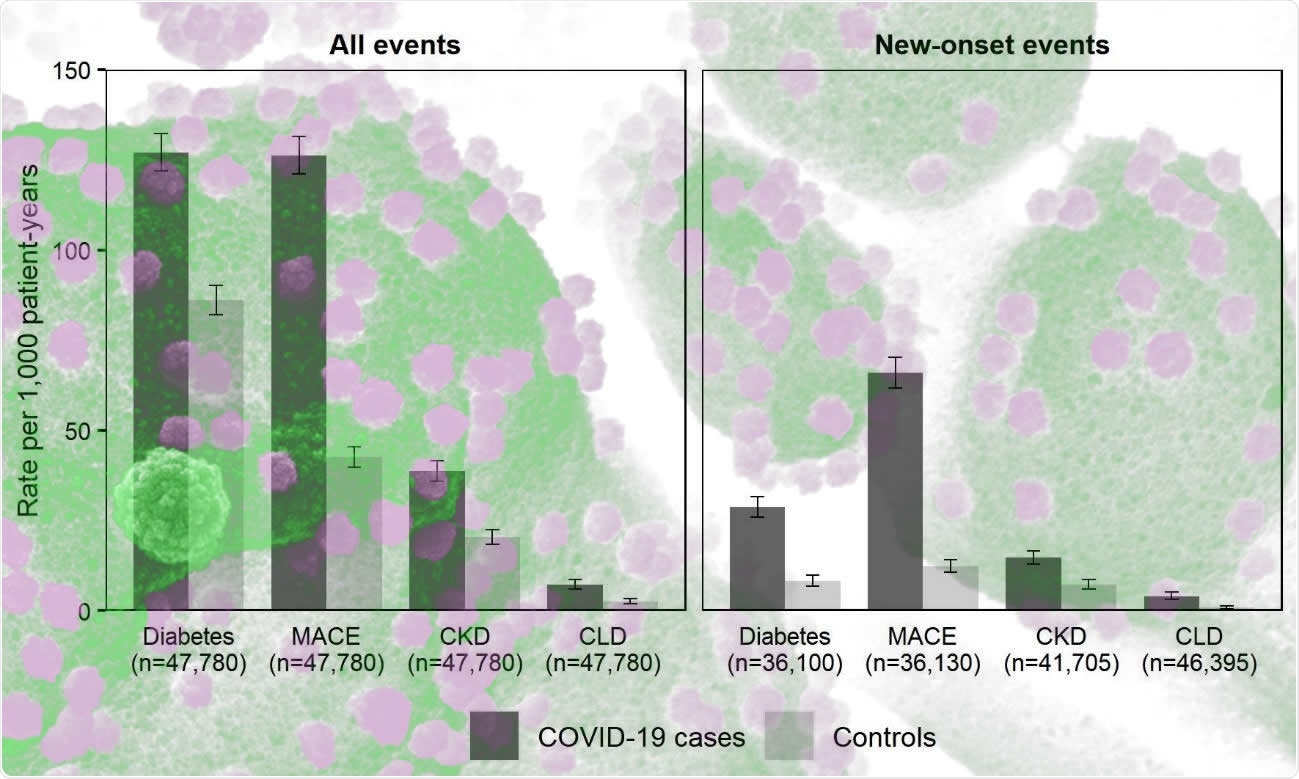
Rates of adverse events contrasting individuals with COVID-19 in England discharged from hospital by 31 August 2020 with matched controls
RRs were higher for individuals aged less than 70 compared to those who were 70 years or above. RRs were also higher in ethnic minority groups compared to the White population. The most significant differences were found in respiratory disease: 10.5 [9.7 to 11.4] for people aged less than 70 years versus 4.6 [4.3 to 4.8] for people who were 70 or above, and 11.4 (9.8 to 13.3) for non-White population versus 5.2 (5.0 to 5.5) for the White population.
"Individuals discharged from hospital following acute COVID-19 face elevated rates of mortality, readmission, and multi-organ dysfunction compared with the background levels that exist for these individuals, and the relative increase in risk is neither confined to the elderly nor uniform across ethnic groups."
Elevated risk of multi-organ dysfunction was not uniform across different ethnicities
Based on the study's findings, the authors concluded that individuals discharged from hospital following a COVID-19 infection have higher rates of multi-organ dysfunction compared with controls rates. Interestingly, the increase in risk was neither confined to the elderly nor uniform across different ethnicities. The diagnosis, treatment, and prevention of long-term complications of COVID-19 requires integrated approaches rather than organ- or disease-specific approaches. According to the authors, there is an urgent need for more research to establish the risk factors for PCS.
"Integrated care pathways are structured, multidisciplinary care plans for specific conditions, which have been effective in other diseases such as chronic obstructive pulmonary disease and may have utility in the management of PCS."

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Epidemiology of post-COVID syndrome following hospitalisation with coronavirus: a retrospective cohort study Daniel Ayoubkhani, Kamlesh Khunti, Vahé Nafilyan, Thomas Maddox, Ben Humberstone, Sir Ian Diamond, Amitava Banerjee medRxiv 2021.01.15.21249885; doi: https://doi.org/10.1101/2021.01.15.21249885, https://www.medrxiv.org/content/10.1101/2021.01.15.21249885v1
- Peer reviewed and published scientific report.
Ayoubkhani, Daniel, Kamlesh Khunti, Vahé Nafilyan, Thomas Maddox, Ben Humberstone, Ian Diamond, and Amitava Banerjee. 2021. “Post-Covid Syndrome in Individuals Admitted to Hospital with Covid-19: Retrospective Cohort Study.” BMJ 372 (March): n693. https://doi.org/10.1136/bmj.n693. https://www.bmj.com/content/372/bmj.n693.