As the coronavirus disease 2019 (COVID-19) pandemic continues to wreak havoc across the globe, scientists race to further understand the virus and how it infects the body. This way, safe and effective therapeutics and other potential preventive measures can be developed to bring surging case-loads across the globe under control.
Caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), COVID-19’s spread has led to the emergence of a new highly infectious variant, the B.1.1.7, which, through increased transmissibility, has contributed to surging cases worldwide. To date, there have been nearly 100 million cases confirmed globally.
Researchers at the Erasmus Medical Centre in the Netherlands and the University of Illinois at Urbana-Champaign in the US found that SARS-CoV-2 rapidly adapts to Vero E6 cell culture propagation and that this can be prevented by using cell lines with an active serine protease-mediated entry pathway. The team also noted that propagating SARS-Cov-2 on the human airway cell line Calu-3, which expresses serine proteases, can help prevent multibasic cleavage site (MBCs) mutation.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
SARS-CoV-2 and mutation
Like any other virus, the SARS-CoV-2 tends to mutate, causing the emergence of new variants.
COVID-19 vaccine development commenced many months ago, and a few vaccine candidates that already been approved for roll out in many countries, including the UK, the US, and Canada.
However, the question of whether or not new variants pose a threat to the current vaccines’ efficacy is still unclear. The continual emergence of new strains, the lack of targeted antivirals, and the adaptive capacity of the virus show that further research into SARS-CoV-2’s viral evolution and its implications on vaccination efforts is crucial.
Laboratory studies
SARS-CoV-2 laboratory studies pave the way for scientists to explore the virus’s structure and how it can affect the body. The first step in most laboratory studies is in vitro virus propagation to get highly concentrated virus stocks.
Despite recent advances in physiologically relevant in vitro cell culture systems, techniques to propagate clinical isolates have not changed to produce progeny viruses after inoculation of these cells with a specimen containing the virus. The most popular cell line in virology is the Vero cell line, which was obtained from the kidney of an African green monkey.
The cell line and its derivatives contain deletions of genes, which works in the antiviral interferon response. Some of the mutations are mostly found in transformed cell lines and open the door for virus replication, producing a high titer virus.
Scientists previously reported that the SARS-CoV-2 MBCs in cell culture have shown that in vitro propagation systems may sometimes fail to show important aspects of the virus life cycle.
Since mutations impact the results and relevance of laboratory experiments with SARS-CoV-2, it is imperative to know why these happen in order to prevent them.
Previous studies have shown that SARS-CoV-2 MBCs boost serine protease-mediated entry. Vero E6 cells, which are commonly used in the laboratory to grow virus stocks, lack this entry pathway, making the virus use another entry point – the endosomal cathepsins.
The team believed that mutations in the MBCs could be averted in cells with an active serine protease-mediated entry pathway.
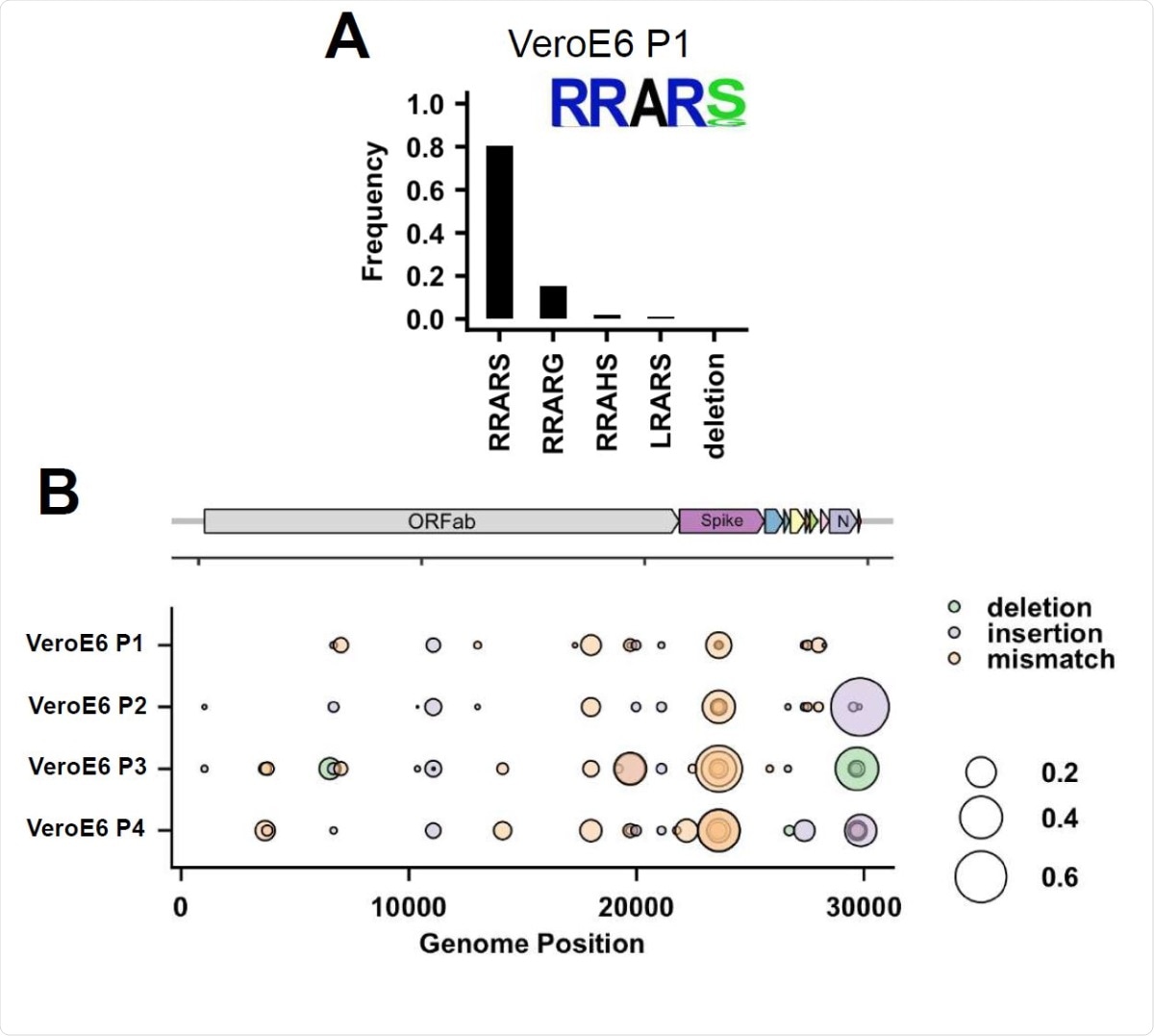
Deep-sequencing analysis of Vero E6 passage 1 virus multibasic cleavage site and full genome deep-sequencing analysis of passage 1-4 viruses. (A) Deep-sequencing analysis of the VeroE6 passage 1 virus stock. In each graph the amino acid sequence logo of the multibasic cleavage site is shown. (B) Full genome deep-sequencing analysis of VeroE6 passage 1, 2, 3 and passage 4 viruses.
The study
In the study, which appeared on the pre-print bioRxiv* server, the researchers state that virus propagation methods use transformed cell lines to grow viruses from clinical specimens, making some viruses rapidly adapt to cell culture conditions, a process helped by high viral mutation rates.
When the researchers propagated SARS-CoV-2 in Vero E6 cells, the virus mutated or deleted the multibasic cleavage site (MBCs) in the spike protein that allows the serine protease to enter human airway cells. The team also noted that propagating SARS-CoV-2 on the human airway cell line Calu-3, which expresses serine proteases, prevented MBCs mutation.
Further, the team also showed that the ectopic expression of the serine protease TMPRSS2 in Vero E6 cells prevented MBCs mutations.
When the team used a human airway organoid-based culture system for viral propagation, the same results came out. Hence, the team recommends that further studies, to develop more in-depth knowledge of this area of viral biology, should be done to help formulate methods to prevent cell culture adaptation.
Alternatively, a 2D airway organoid-based cell culture model can be used for SARS-CoV-2 propagation if in the future new variants emerge that are not genetically stable on Calu-3 cells... Our study also shows that deep-sequencing rather than consensus sequencing of viral stocks is critical for obtaining relevant and reproducible results in SARS-CoV-2 studies,” they added.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Lamers, M., Mykytyn, A., Breugem, T., Wang, Y., et al. (2021). Human airway cells prevent SARS-CoV-2 multibasic cleavage site cell culture adaptation. doi: https://doi.org/10.1101/2021.01.22.427802, https://www.biorxiv.org/content/10.1101/2021.01.22.427802v1
- Peer reviewed and published scientific report.
Lamers, Mart M, Anna Z Mykytyn, Tim I Breugem, Yiquan Wang, Douglas C Wu, Samra Riesebosch, Petra B van den Doel, et al. 2021. “Human Airway Cells Prevent SARS-CoV-2 Multibasic Cleavage Site Cell Culture Adaptation.” ELife 10 (April). https://doi.org/10.7554/elife.66815. https://elifesciences.org/articles/66815.