The COVID-19 pandemic is caused by a beta coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This coronavirus causes an acute respiratory syndrome that was identified for the first time in Wuhan, China, in December 2019. This new zoonotic virus has put the world on alert, rapidly becoming a pandemic.
Clinically, COVID-19 (coronavirus disease 2019) is a heterogeneous disease. The characteristics range from cough, sore throat, fever, myalgia or arthralgia, fatigue, headache, gastrointestinal problems, loss of smell or taste, among other fewer symptoms.
It is essential to identify the risk factors for a quick diagnosis, better follow-up, and prognosis of infected patients. It is established that age and comorbidities (such as diabetes, hypertension, stroke, cancer, kidney disease, and high cholesterol) are risk factors associated with mortality in COVID-19 disease.
A new analysis of COVID-19 patients' laboratory results reveals strong risk-association with hematological values such as leukocytes and neutrophils.
To discriminate between patients with severe and non-severe COVID-19 quickly, researchers from Peru looked for prognostic signatures in the blood samples of COVID-19 patients. Virgilio E. Failoc-Rojas et al. examined laboratory results and clinical prognosis of COVID-19 patients from a hospital in the Peruvian Amazon. The results of this fascinating new study are published on the preprint server medRxiv*.
The researchers found increased levels of leukocytes, neutrophils, low levels of lymphocytes, monocytes, and eosinophils had a strong association with mortality.
"Parameters such as leukocytes and neutrophils were statistically much higher in patients who died."
The study
The study cohort was 127 hospitalized patients from a hospital in Ucayali (located in the Central Jungle, in eastern Peru). All of the patients were confirmed diagnosis of COVID-19 during the period from March 13 to May 9, 2020. COVID-19 confirmation was confirmed via polymerase chain reaction-transcriptase (RT-PCR) assay of nasopharyngeal swab samples and rapid immunochromatographic test. This population saw a mortality of 75 people.
The laboratory evaluations consisted of leukocytes, neutrophils, platelets, RDW-SD (red cell distribution width with standard deviation), RN / L (the neutrophil-lymphocyte ratio), fibrinogen, CRP (C-reactive protein), D-dimer, DHL (Lactate Dehydrogenase), hematocrit, monocytes, and eosinophils.
While the study population had overall high levels of biochemical and hematological values, the researchers stratified unique observations according to mortality.
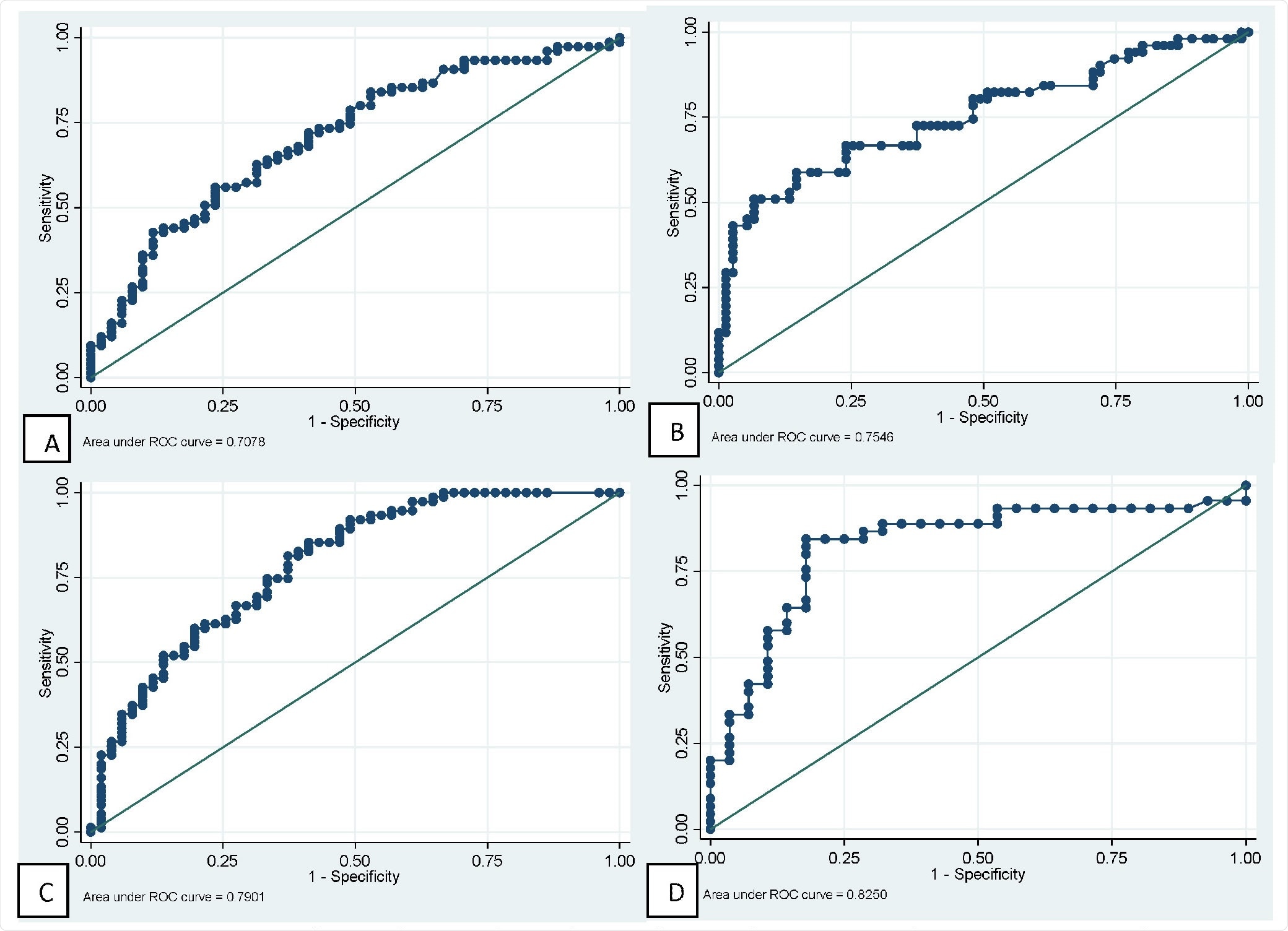
ROC curves of main hematological tests for predicting mortality in patients with COVID-19. A: Neutrophil. B: Lymphocytes. C: Neutrophil / lymphocyte ratio. D: Fibrinogen.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
They found: 1) leukocytes and neutrophils were higher in patients who died 2) they also had lymphocytopenia (abnormally low level of lymphocytes) compared to normal values in survivors (720 vs. 1,360 respectively), and 3) low levels of monocytes and eosinophils.
The researchers also found that other parameters such as the RN / L and fibrinogen were higher in the population that died than those that survived. The observed similar platelet values, red cell distribution width with standard deviation (RDW-SD), and D-dimer, in both groups.
Corroborating with other studies, they observed in this study that for each one-year increase in age, the probability of death increased by 4%.
The IRR (Incidence Risk Ratio) analysis for the numerical variables showed results strongly associated with hematological values such as Leukocytes (scaled by 2,500 units), neutrophils (scaled by 2,500 units); on the contrary, it is observed that the increase of 1,000 units in lymphocytes, the probability of dying decreased by 48%, the researchers write.
Notably, the researchers found the most significant association of D-dimer with death. They found that elevated levels of D-dimer - for each 1 mg / L increase - the risk of dying increased by 25%. D-dimer is a fibrin degradation product indicative of hypercoagulability and thrombotic events.
Conclusion
To date, COVID-19 has claimed over 2.26 million lives out of over 104 million COVID-19 confirmed infections globally. The observations from this study are important to understand the prognosis of patients with COVID-19. This new information may help deliver timely therapeutic support and offer a chance to progress the patients' condition from severe to normal.
It is known that COVID-19 has a significant impact on the hematopoietic system and hemostasis; leukocytosis, lymphopenia, and thrombocytopenia are associated with increased severity and even death in COVID-19 cases. Lymphopenia can be considered prognostic.
This study looks at the biochemical and hematological parameters of COVID-19 patients in association with mortality risk. Against this background, the researchers find diverse parameters that are strongly associated with death.
These observations in COVID-19 patients - severe and non-severe - will help better understand the key traits. Such a study, looking for prognostic markers for varied symptomatic diseases like COVID-19, spearheads future disease research, control, and prevention.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Prognosis and hematological findings in patients with COVID-19 in an Amazonian population of Peru, Sebastian Iglesias-Osores, Arturo Rafael-Heredia, Eric Ricardo Rojas-Tello, Washington A. Ortiz-Uribe, Walter Leveau-Bartra, Orison Armando Leveau-Bartra, Miguel Alcantara-Mimbela, Lizbeth M. Cordova-Rojas, Elmer Lopez-Lopez, Virgilio E. Failoc-Rojas, medRxiv, 2021.01.31.21250859; doi: https://doi.org/10.1101/2021.01.31.21250859, https://www.medrxiv.org/content/10.1101/2021.01.31.21250859v1