Sponsored Content by PittconFeb 24 2021
In this interview, News-Medical Life Sciences talks to Parry Hashemi about the research on in vivo probes for detecting inflammation markers in humans and animals that she will present at Pittcon.
What are some traditional methods for detecting inflammation markers in humans and animals?
Traditionally, a blood or plasma sample will be taken. There are certain proteins that indicate an inflammation; for example, pro-inflammatory cytokines. If the levels of these are raised that corresponds to inflammation.
Other types of markers include histamine, which is relatively simple to measure in blood.
How would you describe the evolution of in vivo technology, including probes, from the past to the present?
People have been interested in measuring things in the brain for a long time, but they did not necessarily have high definition tools until recently.
In animal models, you could extract the whole brain or parts of it and then run a general analysis on the levels of chemicals present. People still do that, but the brain’s functions are very dynamic, and it is very chemically complex.
The things that happen between two cells in the brain will take place within a matter of milliseconds, so determining the overall level of a chemical is not always that informative. Rather, we want to see how that chemical is changing in its native state and that is quite a challenge.
It took scientists quite some time to develop probes that were small enough to implant into the brain without damaging these very fine connections.
This sort of microelectric technology was first developed in the 70s and 80s and then became common in the 90s and early 2000s as faster electrochemical schemes were developed that could take advantage of a certain property of some molecules.
Essentially, electrochemistry involves taking and giving electrons, then getting a signal from a specific molecule.
Most recently, people have started to explore the fluorescent properties of various molecules so that they can engineer ligands and introduce these into the brain. When the ligand attaches to a protein of interest, it fluoresces, and people have designed probes that measure the fluorescence of that ligand. This is a very versatile technique.
Over the past few decades, we have gone from something quite crude - looking at overall levels - to actually defining brain function in real-time.
A lot of this technology is very small; you can put it in the brains of animals and it does not damage any tissues. The animals can exhibit behaviors and you can essentially eavesdrop on their brain as they are doing this.

Using blood samples for the diagnosis of brain disease is problematic due to the blood-brain barrier. Image Credit: decade3d - anatomy online / Shutterstock.com
Can you describe the techniques of using in vivo probes, and why are they useful to biomedicine?
When diagnosing any health issue, one of the first steps is to take a blood sample. This is fine for a lot of diseases of the body, but it does not take into account the blood-brain barrier.
The blood-brain barrier is a strict chemical gateway that controls what goes in and out of the brain. Because of this blood-brain barrier, the levels of things in your blood are not necessarily the same as the levels in the brain. This is compounded by the dynamic nature of brain signals.
Extracting blood from the body does not tell us much about the brain, so it is important to develop appropriate probes specifically for this purpose. In animal models, it is not easy, but it is doable.
However, accessing a human brain is a much more difficult task. Developing the tools and making these smaller, faster and more reproducible in animals is the first step towards being able to investigate these health issues in humans.
One approach we have been working on in my lab is asking questions and exploring these using animals, and then moving to human-like models.
One example of this approach involves stem cell technology and two and three-dimensional stem cell organoids. We can create an in vitro system, use probes to define the chemistry of that system and compare it to what we had previously seen in animals.
This is very powerful because we can use this approach to model diseases and better understand various health aspects of the brain.
The Evolution of In-Vivo Technology
Parry Hashemi Interview _ 2 from AZoNetwork on Vimeo.
Why have you selected in vivo probes for studying neurological systems, and what specific benefits of the probes do you take advantage of in your research?
I have a dual interest - I am interested in the technology as both a chemist and an engineer. I am also interested in trying to measure things that are difficult to measure, and the brain is certainly difficult to measure things in.
On a personal level, the brain fascinates me. We have spent billions of dollars on brain research, but it is still a very enigmatic organ, and we do not know as much about it as we would like.
Neurological disorders and, in particular, psychiatric disorders, are interesting fields. A lot of people do not know this, but depression is the biggest health issue in the world. Around 300 million people are diagnosed with depression worldwide.
To put that number in context, 100 million people are diagnosed with cancer of any kind, so while we think cancer is quite common, depression is at least three times more common. If we think about the stigma and taboo that surrounds depression, the number could actually be much higher than that.
People are saying that post-COVID this is going to get much worse. There is no chemical test for psychiatric illness - you cannot use a blood sample, for the reasons that I mentioned earlier – it is up to the patient to describe their symptoms.
Patients are notoriously bad at doing that, so it is up to the doctor or the healthcare practitioner to base their diagnosis on information from a patient – there is no diagnostic tool for this.
Current therapies are prescribed to a phenomenal number of people, but the way they work or even if they work is under scrutiny because we do not have any way to assess this or look at ways to improve them.
This combination of factors prompted me to think about using our technology to ask some fundamental questions about these things. These psychiatric illnesses are very complicated, so it is impossible to cover the whole spectrum of what is going on, but we could start with something simple.
We said, "Let's choose a molecule that we think is important in depression or psychiatric illnesses and measure it." That is a real feat in itself, but once you do that and you can make a measurement, you can start asking more complicated questions.
For example; How is this involved in this psychiatric illness? How has this involved in depression? What is this drug doing? How can we make this drug better?
We are using basic engineering and chemical technology to take measurements and answer a very big question. It is exciting and challenging, and a lot of different aspects come into it, but I would not have it any other way.
Inflammation is an immune response when a human or animal’s biological system is fighting against harmful agents and attempting to heal itself. What makes inflammation a specifically useful target for biomedical research?
Inflammation is a hot topic and we are realizing that inflammation underlines a lot of health issues, whether gut inflammation, any sort of allergic reaction or a chronic illness. Inflammation is essentially a blanket term for an immune response.
People in my field accept that where there is depression, there is inflammation, and where there is inflammation, there is depression – they are comorbid.
We recently conducted an experiment that we are about to publish. We took a mouse and we induced a localized inflammation in the mouse's body. It is a paradigm that involves a molecule called LPs – lipopolysaccharide - the protein found in the outer membrane of gram-negative bacteria.
As soon as this protein enters the body, there is a strong, acute immune reaction, but as a molecule, it is far too big to get through the blood-brain barrier.
We gave this to mice, and then we measured their brain chemistry. Within minutes, the chemistry of the brain changed in response to this infection or immune reaction. This is really fascinating because people with chronic illnesses like diabetes, obesity or cancer experience depression at a much higher rate than the general public.
For a long time, people had put it down to the fact that it is depressing to have a chronic illness, psychologically, but I think we are realizing that it is not just a psychological reaction to having a chronic illness – there is a physiological reason behind it.
The same principle applies to gut inflammation. There is a huge field of study that is looking at the gut-brain connection, working with people that have depression and looking at their gut bacteria to better understand what that connection is.
For psychiatric illnesses, we are just starting to appreciate the role of the immune system and how important this is in controlling our moods and our cognitive abilities.
A new area of study is looking into the gut-brain connection and how gut bacteria may be connected to psychiatric disorders. Image Credit: Anatomy Image / Shutterstock.com
Can you describe your research on in vivo probes for detecting inflammation markers in humans and animals that you are presenting at Pittcon?
We discovered that inflammation has an effect on the brain and that if you are experiencing inflammation, the serotonin levels in the brain are reduced – something long associated with depression. We were not surprised that we saw serotonin levels go down, but then we began to ask why.
To help answer this question, we focused on another messenger - histamine. Histamine is a very strong messenger of inflammation in the body, commonly associated with allergies.
We know we can measure histamine, and we also know there is histamine in the brain, but we do not know much about what it is doing there.
We became interested in histamine because it is important in inflammation in the body, but also because serotonin neurons in the brain have histamine receptors on them, and this system of receptors is inhibitory. If histamine in the brain was to increase because of the way these neurotransmitters interact, then serotonin would decrease.
We developed new technology to measure histamine in the brain; we defined it and characterized it in great detail, exploring how it is controlled, released and re-uptaken.
Next, we induced inflammation to examine the comodulation of serotonin and histamine. We hypothesized that during inflammation, the histamine levels in the brain go up and force the serotonin down.
Rather than targeting serotonin pharmacologically, we have been targeting histamine, and we have actually had much better results in terms of getting serotonin levels back to normal by managing histamine rather than serotonin itself.
How is measuring inflammation markers like neurotransmitters shaping ideas of health?
I think we now have a good understanding of what is happening in the brain, in animal models during inflammation.
Next, we want to explore this using human or human-like models. My dream would be to be able to get some sort of accessible marker from the body and to use this to develop a chemical diagnosis of what is going on in the brain.
There are a lot of inflammation markers in the body and a lot of signaling molecules that are involved in the immune system.
Our immune cells signal with histamine, so looking at these and trying to characterize them may be a step towards finding that mirror in the body that tells us about the brain, and then better diagnosing and better designing treatment strategies.
3D illustration of a mast cell releasing histamine, a key signaling molecule, an inflammation marker. Image Credit: Kateryna Kon / Shutterstock.com
How does your work apply to the current understanding of the brain and neurodegeneration, stress, and toxins?
Neurodegeneration is a broad field, and different neurodegenerative diseases are defined by different phenotypes. What they all have in common is a high comorbidity of depression.
They also have an inflammation aspect to them and we think that the depression that underlies neurodegeneration might really be a consequence of the inflammation.
Another compounding aspect is that some of the pharmaceutical therapies for neurodegeneration will detrimentally target serotonin or histamine. We did not know this until very recently, but this interlink between the phenotype of the neurodegeneration, the inflammation and the various drugs is multifaceted.
Can you give some insight into your lab approaches for designing and engineering novel analytical microdevices to measure messengers like neurotransmitters?
We are doing a lot of different things, so we are using different techniques and different principles. In my lab, we have neuroscientists, chemists and engineers. We also have people with mathematical and theoretical backgrounds.
We work collaboratively, engaging in the broader community with clinicians, neuroscientists, physiologists, mathematicians and statisticians. We have to bring together a lot of different disciplines to answer the kind of questions that we are asking.
When we decide we want to develop a tool to measure a particular neurotransmitter, we start by designing different electrodes or different probes. We design the tool, make it and start by characterizing it in a beaker, out of the brain. Next, we put it in the brain and note the different issues that come up.
The process is iterative, so at this point, we will go back to the drawing board, redesign the tool and make it smaller and/or faster. We might have to modify it to give it more selectivity. We also have to develop calibration, processing and data analysis systems to accurately tell us what that signal means.
The final part of this work involves expanding our capabilities to other molecules. I have talked about serotonin and histamine in my lab, but we are interested in others too.
Properly interpreting data from our probes requires a different set of skills. We work with brilliant neuroscientists who know about receptors, so once we have the signal, we can say, "Look, at this signal - we did this, and it went up, then we didn't, and it went down. What do you think it means?"
They help us formulate hypotheses, which we can come back and test.
Finally, when we have a hypothesis and appropriate data, we will work with the mathematicians to start making models that dimensionally describe these processes. We can feed these models with more experiments, and the models can tell us whether or not we have to do more experiments. Again, this is an iterative process.
We also work with drug designers. We give them information about what we found and what we think needs to happen, and they design drugs based on this. We use those drugs to see if we can develop better antidepressants.
We even work with human clinicians to access things in the body that will tell us about the brain. Overall, we go from very basic engineering and chemistry through the whole spectrum to human clinical practice.
Neurotransmitters such as serotonin, dopamine, and histamine are linked with mood and emotions and are thus vital to focus on when studying depression. What other applications for biomarkers and probes would you like to see in the coming years?
I would love to start using probes in the gut to explore the gut-brain connection that I was talking about.
There is a nerve that connects the brain and the gut, and people think that it is serotonergic in nature. It would be fascinating to study that connection because I think we have a very clear connection between our thoughts and emotions and the way our bodies react to them.
The bacteria in our gut may drive our behavior more than we ever gave it credit for. For example, when we crave a certain food, we do not know if it is us craving it, or if the bacteria in our gut is craving it because they have their own nutritional requirement.
People are also putting probes in all sorts of interesting places, like lymph nodes, kidneys and arteries. The possibilities are endless.
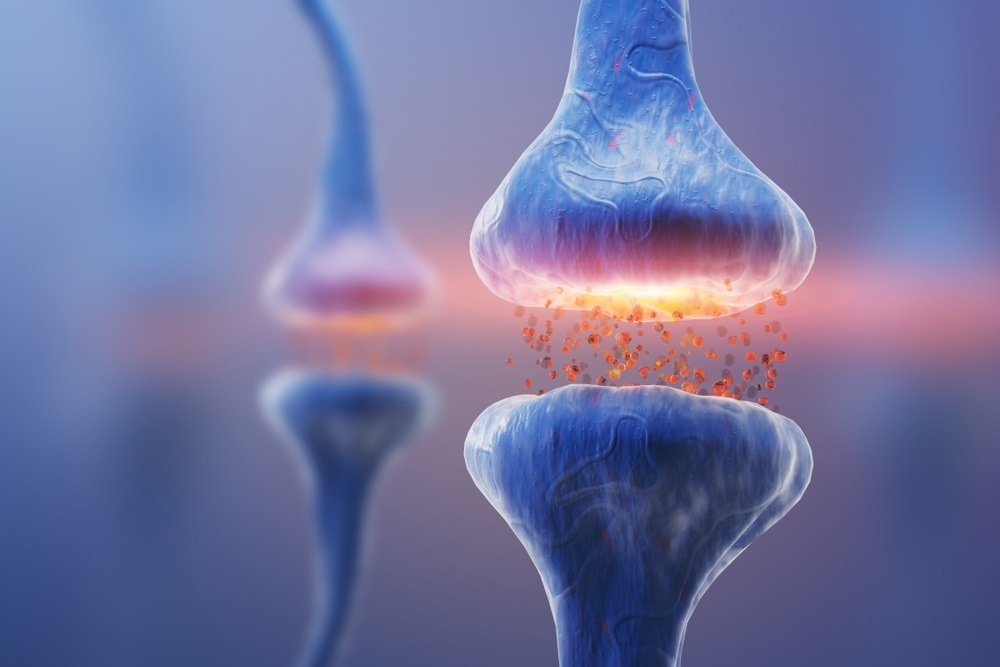
Neurotransmitters such as serotonin, dopamine, and histamine are linked with mood and emotions. Image Credit: KateStudio / Shutterstock.com
What does the future hold for you and your research in neural engineering?
My five to ten-year plan is to start pushing ahead with chemical diagnostics for depression. I think it is time - we are in a bad place with the number of diagnoses of depression, and it is going to get worse.
We need a good, robust way to diagnose depression and to screen new drugs. We also need a good, robust way of treating people on a personal, individualistic level because everyone’s inflammation is different.
We are making chips, we are making devices, we are taking different types of cells from the body and we are asking, "Can you be found in the brain? Can you give us information about the brain? And if so, can we use you to screen drugs?"
Our ultimate goal is to develop a user-friendly platform that we can make available to doctors and healthcare practitioners so that they could use it themselves.
What influence do events like Pittcon have on the publicity and direction of your research?
Pittcon is a brilliant forum. It is our favorite conference, and we get a lot of exposure out of it because so many different types of people with different interests are in attendance. Because we bridge multiple disciplines, we get to interact with key players in various fields.
It is good to see my students give talks, and I usually give a couple of talks too. It is also great to see what is happening on the cutting edge of analytical chemistry and seeing what people are doing in the brain with different techniques. We have had so many collaborations and long-standing relationships come out of attending Pittcon.
Pittcon will be virtual and will be different this year. What is the importance of still staying connected with other researchers and attendees even online?
Things have slowed down, but we have still been doing research and we still have new and exciting work to share. We have gotten used to seeing each other once a year, sharing ideas and working on collaborations, so I think it is important that we continue to do this, even if it's in a virtual format.
I am really looking forward to it because these are people I have not seen for a long time. I think just from a psychological perspective. It will be great to see their faces, hear about their work, and get some normality back. When March arrives, it is Pittcon time; come rain or shine. I think that it is a good thing.
About Pittcon
 Pittcon® is a registered trademark of The Pittsburgh Conference on Analytical Chemistry and Applied Spectroscopy, a Pennsylvania non-profit organization. Co-sponsored by the Spectroscopy Society of Pittsburgh and the Society for Analytical Chemists of Pittsburgh, Pittcon is the premier annual conference and exposition on laboratory science.
Pittcon® is a registered trademark of The Pittsburgh Conference on Analytical Chemistry and Applied Spectroscopy, a Pennsylvania non-profit organization. Co-sponsored by the Spectroscopy Society of Pittsburgh and the Society for Analytical Chemists of Pittsburgh, Pittcon is the premier annual conference and exposition on laboratory science.
Proceeds from Pittcon fund science education and outreach at all levels, kindergarten through adult. Pittcon donates more than a million dollars a year to provide financial and administrative support for various science outreach activities including science equipment grants, research grants, scholarships and internships for students, awards to teachers and professors, and grants to public science centers, libraries and museums.
Visit pittcon.org for more information.