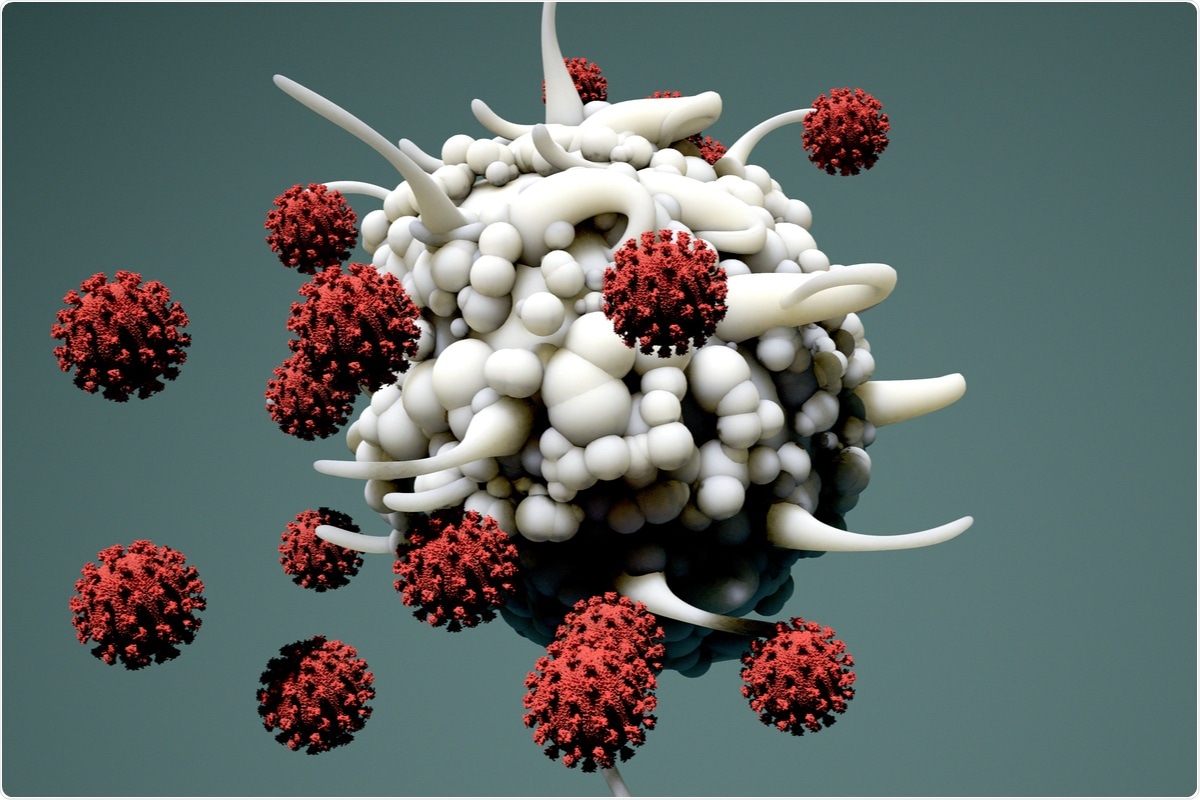
Dendritic cells play a pivotal role in the immune response through their involvement in antigen presentation, cytokine production, and immune cell recruitment. Coronavirus Disease 2019 (COVID-19) patients often express dendritic cell deficiency, possibly due to mass migration of these cells to the lungs and other sites of inflammation. Dendritic cell depletion is associated with lower interferon production and poorer prognosis from SARS-CoV-2 infection, and could potentially linger for a significant period of time following recovery from COVID-19, leaving a patient vulnerable to other pathogens. In a new study, recently released on the bioRxiv* preprint server, the persistent influence of SARS-CoV-2 on dendritic cell deficiency seven months post-infection is asserted, and the mechanism of action investigated.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
How does SARS-CoV-2 affect dendritic cells during infection?
Dendritic cells are divided into categories based on function, two of which are: myeloid dendritic cells, which regulate pro-inflammatory responses; and plasmacytoid dendritic cells, which produce type I interferons. Plasma was collected from acutely infected COVID-19 patients and compared with controls, revealing that the population of both types of dendritic cell were significantly lower amongst the infected.
As plasmacytoid dendritic cells are known to be primary producers of interferon in SARS-CoV-2 infection the group also investigated the production of this molecule in both COVID-19 patients and healthy donors, noting a positive correlation between the dendritic cells and interferon levels.
Biomarkers that indicate dendritic cell activation were then measured in the patient samples, finding that most of the biomarkers investigated were notably downregulated while one was upregulated, and suggesting that homing and activation patterns for dendritic cells are altered by SARS-CoV-2 infection.
The group then quantified the population of dendritic cells and their related biomarkers amongst mild and severe COVID-19 patients, finding that there was only a mild but positive correlation between disease severity and dendritic cell deficiency. Interferon production was, however, very notably reduced by the severity of the condition. Additionally, the ratio between the various dendritic cell homing and activation molecules investigated varied by disease severity in a differential manner, with some aspects, again, being up- or downregulated. Generally, however, the group concludes that the disruption of the biomolecular signaling system is strongly associated with the level of inflammatory response experienced by a patient.
Dendritic cell involvement in long COVID
Patients that had recovered from COVID-19 around seven months earlier, some of which had been hospitalized, were also included in the study. Overall, a higher percentage of myeloid dendritic cells were observed in those previously hospitalized compared to healthy volunteers, with variation amongst the various sub-forms. Plasmacytoid dendritic cells remained highly depleted, while interferon production was also impaired most greatly among the hospitalized compared to the non-hospitalized, which was higher still than the healthy subjects. Dendritic cell activation and homing markers were also compared amongst these groups, generally showing similar dysregulation as previously reported, with most molecules being strongly downregulated while selected others exhibited upregulation, seen most strongly amongst the hospitalized.
Altered interferon production has previously been correlated with severity of SARS-CoV-2 infection, and this association is reinforced by this study. Besides interferon, dendritic cell and activation marker number have been correlated with cytokine levels, particularly that lower dendritic cell presence is associated with higher levels of interleukin-6, where high levels of this biomolecule are also associated with poorer prognosis. Importantly, the group found that the percentage of dendritic cells expressing integrin β7 in peripheral blood was negatively correlated with cytokine levels. Integrin β7 is involved in the localization of dendritic cells. The group suggests that the lower levels of this protein in peripheral blood dendritic cells could imply the mass migration of dendritic cells to inflammation sites. In other words, the large absence of dendritic cells in peripheral blood is due to the majority of these cells, which bear integrin β7, migrating to the lungs.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources