The coronavirus disease 2019 (COVID-19) is a heterogeneous disease caused by the novel betacoronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A significant number of SARS-CoV-2 infections, however, occur without any evident symptoms.
In such asymptomatic cases, the role of humoral immunity is unclear. Are antibodies elicited from asymptomatic cases? And, if so, how long do they last?
To address some of these pressing questions, a team of researchers recently compared antibody responses in 405 asymptomatic individuals with 459 symptomatic COVID-19 patients. They found that IgM responses rapidly declined in both groups. However, they found striking differences concerning the strength and persistence of SARS-CoV-2-specific IgG responses. The team has released their results on the bioRxiv* preprint server.
The IgG responses (both prevalence and durability) and neutralizing capacities correlated positively with the COVID-19 symptoms. Particularly, those antibodies recognizing the RBD (receptor-binding domain) of the S (Spike) protein of SARS-CoV-2, which comprise neutralizing IgG molecules.
The researchers noted that regardless of sex, age, and body weight, asymptomatic individuals lost their SARS-CoV-2-specific IgG antibodies more often and rapidly than symptomatic patients. The results suggest that a considerable fraction of asymptomatic natural infections stimulate a humoral immune response conferring the ability to resist reinfections.
The findings are important for understanding the immunity against SARS-CoV-2 and for designing immunization programs including individuals after asymptomatic infections.
The study cohort involved individuals enrolled in a surveillance program in Wuhan, China. The researchers tested the plasma levels of immunoglobulin G (IgG) and M (IgM) against the viral spike or nucleoprotein. The well-defined duration of the SARS-CoV-2 endemic in Wuhan allowed this study to conduct a side-by-side comparison of antibody responses following symptomatic and asymptomatic infections without subsequent antigen reexposure.
In the study, the researchers speculated why the early symptoms correlate with the strength and sustainability of IgG responses: patients with severe infections may produce higher levels of antibodies during the early disease stage because of the stimulation of a large number of antigens and B cell responses outside germinal centers.
Interestingly, the researchers observed that the duration of viral RNA shedding seems to be shorter in asymptomatic people.
This explains a shorter virus replication phase may be associated with an antigen availability that is simply not long enough to prime optimal B cell and/or antibody responses,” the researchers noted.
The researchers also discussed other possible explanations for early symptoms and strong, long-lasting IgG responses: 1) the association between innate immune responses and symptoms, as opposed to innate immune responses and antibody responses; and 2) the overlapping dependence on interferons, which enhance antibody responses and induce class switching.
Since interferon induction is stimulated by viruses, the first explanation (prolonged virus replication) and the second explanation (increased interferon induction) are by no means mutually exclusive.”
Similar to other acute viral infections, the researchers observed that the antibody response dynamics exhibited detectable neutralizing activity half a year after the end of the epidemic and in the absence of additional antigen exposure in nearly half of all asymptomatic individuals.
Although several studies have reported an association between higher viral loads with more severe symptoms, those studies found little to no difference in the virus loads between pre-symptomatic, asymptomatic, and symptomatic patients.
The researchers discussed the limitations of their study: recall bias of asymptomatic carriers due to the delay in the study, a fraction of asymptomatic patients may be missed due to undetectable IgG-S levels, only 20 enrolled asymptomatic individuals, who mounted a detectable antibody response, etc.
The researchers have devised an unprecedented study design dealing with the aftermath of a COVID-19 endemic. Because of the uncertainty in the timing of asymptomatic infections, and the immunity wanes over time, it is an insightful study into determining the prevalence and kinetics of binding and neutralizing antibodies in asymptomatic individuals.
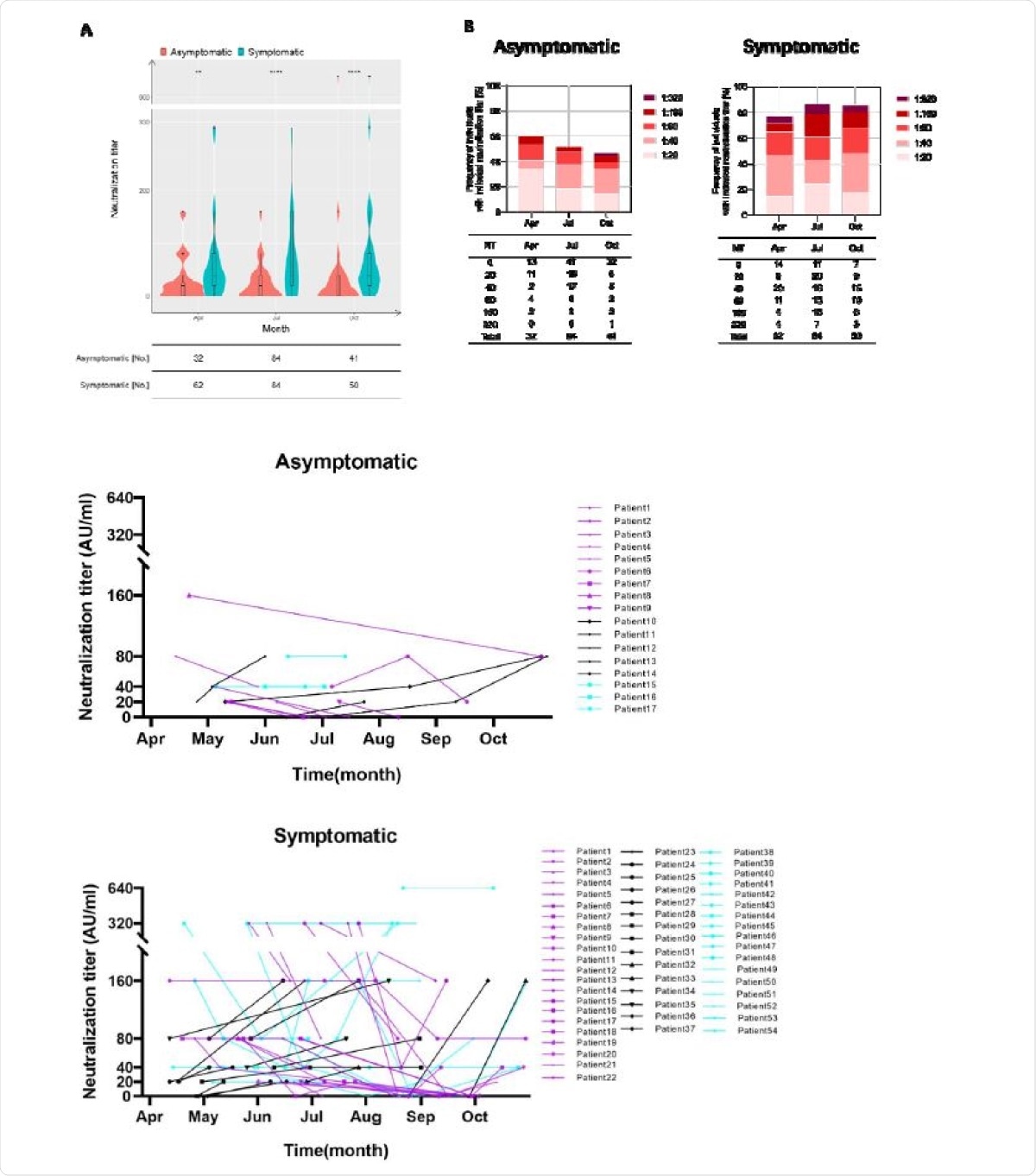
Neutralization activity is defined by the occurrence of symptoms. A, Violin plots show the distribution of neutralization titers of sera derived from derived from asymptomatic individuals (red) and symptomatic patients (blue) during April and October 2020. Boxes depict medians (middle line), 75% quartiles (upper bound), and 25% quartiles (lower bound). Whiskers indicate 1.5-times interquartile ranges above and below boxes. The table below the figure highlights the number of clinical specimens that have been assessed. Statistical analysis was performed by two-tailed Mann-Whitney U test. Asterisks depict levels of significance as follows: ns, not significant (p=0.05); *p<0.05; **p <0.01; ***p<0.001. B, like in ‘A’ but the frequencies of individuals exhibiting indicated neutralizations titers are depicted. C, Sequential sampling and analyses of neutralization activity in 17 asymptomatic individuals and 54 symptomatic COVID-19 patients. Different colours highlight different trends as follows: purple: declining trend; black: increasing trend; light blue: unchanged neutralization.
In the study, the authors claimed that this is the first comprehensive side-by-side comparison of asymptomatically infected individuals and symptomatic COVID-19 patients in the aftermath of a SARS-CoV-2 epidemic.
Half a year after the Wuhan COVID-19 epidemic ended, although asymptomatic individuals had lower IgG-S antibody titers, positivity rates, and neutralizing activities compared to symptomatic patients, nearly half of asymptomatic subjects had sufficient neutralization activity, the researchers concluded in the study.
Despite this good news, above mentioned disparity in the strength and duration of IgG-S responses raised by symptomatic and asymptomatic infections, strongly argue in favour of vaccine programmes including individuals who underwent asymptomatic SARS-CoV-2 infections, ideally with an intermediate prioritization adjusted between vulnerable uninfected individuals and symptomatic COVID-19 patients.”
Journal reference:
- Jun Wu, Bo-Yun Liang, Yao-Hui Fang, Hua Wang, Xiao-Li Yang, Shu Shen, Liang-Kai Chen, Su-Meng Li, Si-Hong Lu, Tian-Dan Xiang, Jia Liu, Vu Thuy Khanh Le-Trilling, Meng-Ji Lu, Dong-Liang Yang, Fei Deng, Ulf Dittmer, Mirko Trilling, Xin Zheng. (2021). Occurrence of COVID-19 symptoms during SARS-CoV-2 infection defines waning of humoral immunity. bioRxiv 2021.03.26.437123. doi: https://doi.org/10.1101/2021.03.26.437123, https://www.biorxiv.org/content/10.1101/2021.03.26.437123v1